Heart:房颤合并慢性肾脏病人,如何使用华法林及抗凝管理?
2017-05-23 cailingrui MedSci原创
慢性肾脏疾病(CKD)常与心房颤动(AF)风险增加相关。在美国,需要透析治疗的慢性肾病患者中约有10%被诊断出有房颤,而实际上这个合并房颤的病人可能高达40%。 在房颤病人中,合并慢性肾病会增加中风的危险,慢性肾病本身也会提升病人的房颤血栓危险度评分(CHADS2 score)。另一方面,华法林和慢性肾病都会增加房颤病人的出血风险。慢性肾病可以同时增加中风和出血的危险,它对房颤的疾病管理
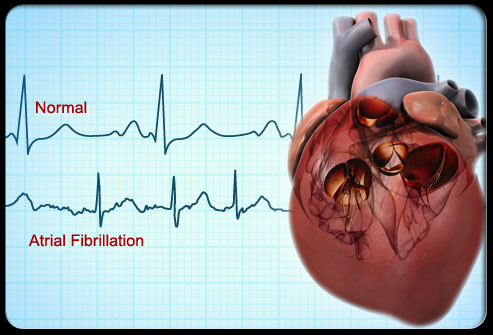
慢性肾脏疾病(CKD)常与心房颤动(AF)风险增加相关。在美国,需要透析治疗的慢性肾病患者中约有10%被诊断出有房颤,而实际上这个合并房颤的病人可能高达40%。
在房颤病人中,合并慢性肾病会增加中风的危险,慢性肾病本身也会提升病人的房颤血栓危险度评分(CHADS2 score)。另一方面,华法林和慢性肾病都会增加房颤病人的出血风险。慢性肾病可以同时增加中风和出血的危险,它对房颤的疾病管理带来的影响还未完全阐明。华法林治疗的慢性肾病患者的中风和出血风险增加可能是由于抗凝管理,也就是凝血酶原时间的国际标准化比值(INR)监控不利导致的。
作者对美国退伍军人管理局(VA)医疗体系中新发的房颤病人做了回顾性队列研究。评估了并发慢性肾病患者华法林用药的抗凝作用,INR监测以及服药期间和之后达到目标INR的百分比(TTR)。在123,188房颤病人队列中,合并严重慢性肾病的患者中华法林使用减少(57.2%–46.4%),低于接受透析治疗的病人(62.3%)。在相同INR监控的情况下,TTR≥60% 的比例随着CKD患者严重程度增加而降低,在透析病人中只有21%可以达到TTR≥60%。 透析病人出现INR <1.5 或 >3.5的频率最高 (30%),其中INR >3.5(12% ),更有低TTR持续长达3年之久的情况。
研究展示了房颤合并慢性肾脏病人华法林使用后,抗凝作用的巨大差异性。中晚期CKD病人,包括接受透析治疗的患者都有不同程度的TTR减少的情况,抗凝控制效果不佳。研究结果显示,更加频繁的抗凝管理监控用药,或采用直接口服抗凝药的替代疗法可能会对房颤合并慢性肾脏病人的治疗有帮助。
原始出处:
Yang, Felix, et al. Warfarin utilisation and anticoagulation control in patients with atrial fibrillation and chronic kidney disease. Heart (2016): heartjnl-2016.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












不错的方式,努力学习,刻苦专研,不断总结出来新经验。给点个赞!
96
#ART#
60
#HEART#
74
#慢性肾脏#
72