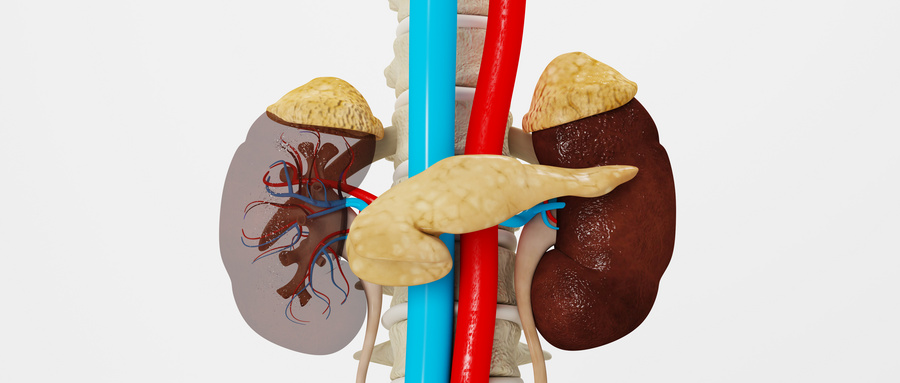
系统性红斑狼疮对肾脏的影响
2021-09-03 xiangting MedSci原创
系统性红斑狼疮(SLE) 是一种侵犯全身结缔组织的自身免疫性疾病,LN通常发生在SLE病程的早期。
系统性红斑狼疮(SLE) 是一种侵犯全身结缔组织的自身免疫性疾病, 常会出现肾脏受累,称为狼疮性肾炎(LN),表现为蛋白尿、血尿、肾功能不全等,LN通常发生在SLE病程的早期。
1. LN的发病机制 虽然LN被视为一种典型的免疫复合物肾小球肾炎,但LN的发病涉及多种机制,其中包括:基因表达导致中性粒细胞活化、基因表达导致髓系和其他免疫细胞群中干扰素和其他促炎症介质增加、中性粒细胞胞外诱捕网(NET)释放以及补体活化。SLE及其他免疫复合物介导的肾小球疾病中的肾小球损伤模式主要与免疫沉积物的形成位置有关,免疫沉积物主要由抗dsDNA引起。
2. LN的临床表现 LN患者最常见的异常为蛋白尿。其他常见的临床表现包括:镜下血尿伴或不伴红细胞管型、肾功能损害、肾病范围蛋白尿或肾病综合征及高血压。
3.LN的诊断 对于SLE患者,如果尿沉渣镜检有活动性发现[持续性血尿(每高倍镜视野中≥5个红细胞)和/或细胞管型]、蛋白尿和/或血清肌酐升高(或eGFR降低),应考虑LN。抗dsDNA抗体滴度高及补体(C3和C4)水平低常提示活动性SLE,此时应考虑到LN可能。LN也是部分SLE患者的首发症状。诊断LN的金标准是肾活检。肾活检是确定肾脏受累性质、排除肾脏损害的其他原因、确定LN组织病理学亚型以及评估疾病活动性和慢性程度的关键。
4.LN的分型 目前广泛使用的分型根据肾活检结果将SLE相关性肾小球疾病分为6种类型,其中包括:轻微系膜性LN(Ⅰ型)、系膜增生性LN(Ⅱ型)、局灶性LN(Ⅲ型)、弥漫性LN(Ⅳ型)、狼疮膜性肾病(Ⅴ型)及晚期硬化性LN(Ⅵ型)。
5. 其他类型的狼疮性肾脏病变 LN除了肾小球病变以外,还有其他类型的狼疮性肾脏病变,其中包括:肾小管间质性肾炎、血管病变(包括血栓性微血管病)、狼疮性足细胞病变、塌陷型肾小球硬化,以及少数病例中的药物性狼疮相关肾脏病。许多这些肾脏损伤模式仅能通过肾活检确诊。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#系统性#
44
#狼疮#
54
#红斑#
43
学习了,
84