用心脏超声这样测肺动脉压,可媲美右心导管
2019-07-29 卢芳 中国循环杂志
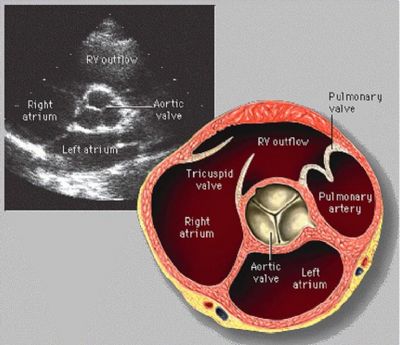
一说肺动脉高压,通常都会想起诊断金标准右心漂浮导管,用超声心动图来诊断,很多研究结果表明有点“水”,不过超声心动图真的就“扶不上墙”?
近日,重庆医科大学附属第一医院游小钧、董倩等对常规的超声心动图测量方法“动了动手”,结果显示,校正后超声心动图法测量肺动脉压力是个好办法,与右心漂浮导管法的测量值接近,较有临床价值。
据悉,通常超声心动图评估肺动脉压力是通过三尖瓣反流和肺动脉瓣反流的多普勒测算的:
肺动脉收缩压≈右心室收缩压=4×(三尖瓣反流峰值速度)2+右心房压;
肺动脉平均压=4×(肺动脉瓣反流早期峰值速度)2+ 右心房压;
肺动脉舒张压=4×(肺动脉瓣反流晚期峰值速度)2 + 右心房压。
研究者在考虑校正超声心动图测量方法时,主要瞄准了两个指标:肺动脉过瓣压和右心房压。
研究者认为,以上传统公式测算肺动脉压忽略了肺动脉瓣过瓣压,且右心房压常采用正常右心房压平均值 10 mmHg,常低估或高估右心房压,考虑用中心静脉压代表右心房压。因此,将上述公式优化为如下:
肺动脉收缩压=4×(三尖瓣反流峰值速度)2+ 中心静脉压-肺动脉瓣过瓣压;
肺动脉平均压=4×(肺动脉瓣反流早期峰值速度)2+ 中心静脉压-肺动脉瓣过瓣压;
肺动脉舒张压=4×(肺动脉瓣反流晚期峰值速度)2+ 中心静脉压-肺动脉瓣过瓣压。
如此这般校正后,研究者在30例接受右心漂浮导管检测肺动脉压力的患者中,在同一天行超声心动图进行了验证和比较。
结果显示,未校正超声心动图法与右心漂浮导管法比较,上述三个值差异较大,而“动了手”的超声心动图法所测则与金标准的差异无统计学意义,而且更接近金标准,相关性更高( r=0.95、0.91、0.96)。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#右心导管#
79
#动脉压#
64
#肺动脉压#
92
#心脏超声#
119
不错
116