Hepatology:绝经后妇女循环性类固醇激素的浓度与肝癌之间的关联
2020-09-09 MedSci原创 MedSci原创
在几乎所有国家,男性肝癌(LC)的发病率均比女性高100%-200%。但是,这种差异主要是由肝细胞癌(HCC)驱动的,其占肝癌病例的75%,肝内胆管癌(ICC)占病例的12%,男性的比率仅高30%。
背景及目的:
在几乎所有国家,男性肝癌(LC)的发病率均比女性高100%-200%。但是,这种差异主要是由肝细胞癌(HCC)驱动的,其占肝癌病例的75%,肝内胆管癌(ICC)占病例的12%,男性的比率仅高30%。本项研究假定激素是性别差异的基础,研究人员通过调查诊断前的循环激素和性激素结合球蛋白(SHBG)水平来判断是否与LC风险相关。
方法与结果:
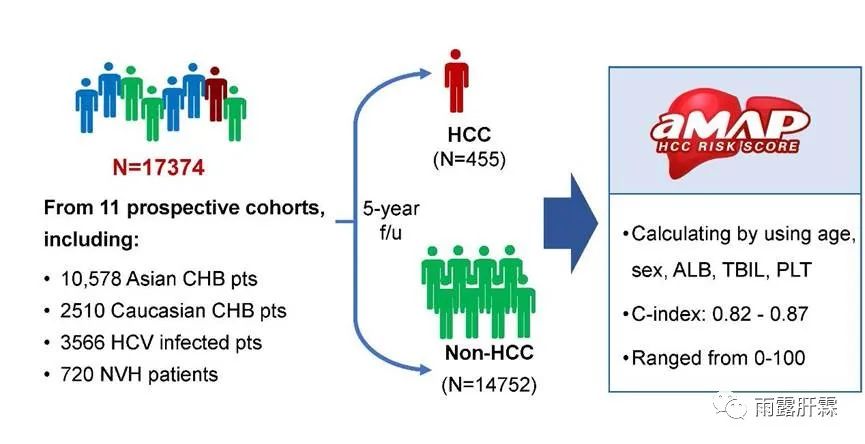
研究人员使用气相色谱/串联质谱法和竞争性电化学发光免疫分析法分别从191名绝经后女性LC患者(HCC,n = 83; ICC,n = 56)和426个对照组的基线血清/血浆样品中定量了7种性甾体激素和性激素结合球蛋白(SHBG)。然后对所有患者的激素水平与肝癌的发生情况进行了统计分析。
结果:
研究结果显示4-雄烯二酮(4-二酮)的浓度增加一倍可降低50%的LC风险(OR = 0.50; 95%CI = 0.30-0.82),而SHBG升高则可提高31%的风险(OR = 1.31; 95%CI = 1.05-1.63)。检查组织学,雌二醇加倍与ICC风险增加40%有关(OR = 1.40; 95%CI = 1.05-1.89),但与HCC无关(OR = 1.12; 95%CI = 0.81-1.54)。
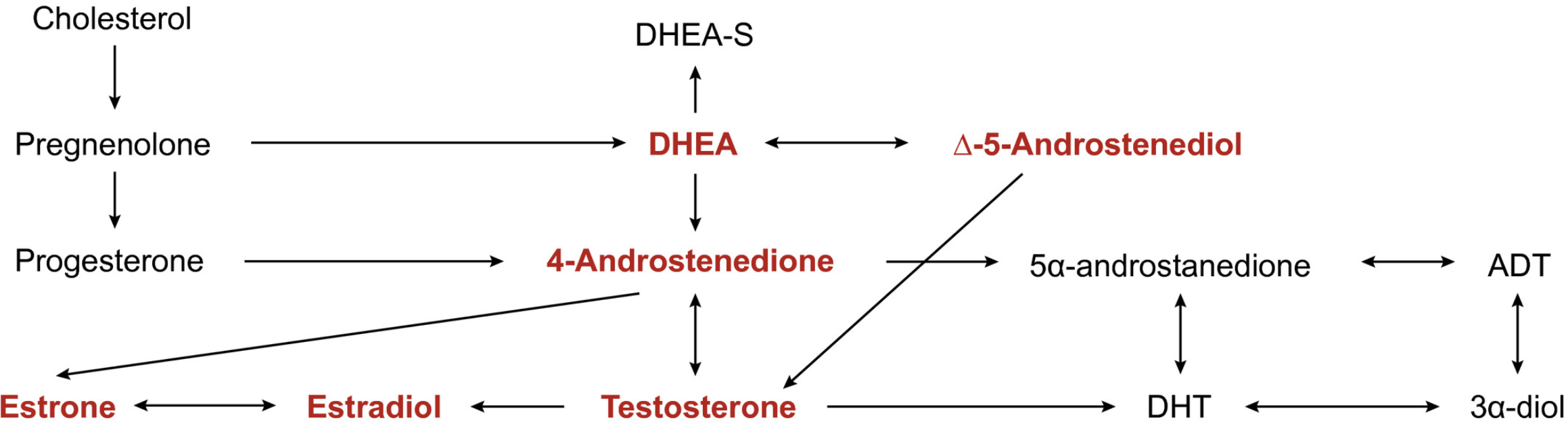
图:类固醇激素代谢途径
结论:
这项研究提供的证据表明,较高的4-二酮水平可能与较低的女性SHBG和较高的LC风险有关,因此女性类固醇激素-雌二醇可能与ICC风险增加有关。
原始出处:
Jessica L. Petrick. Et al. Associations Between Prediagnostic Concentrations of Circulating Sex Steroid Hormones and Liver Cancer Among Postmenopausal Women. Hepatology.2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#类固醇激素#
53
#绝经#
51
#类固醇#
49
#绝经后妇女#
57
#EPA#
46
#浓度#
0
#绝经后#
48
肝癌,接下来就要细分了,对于体质好的病人,能否将PD-1类+抗血管新生+放疗等相结合,甚至有必要用TACE进行减负
61
学习
93
阅读
101