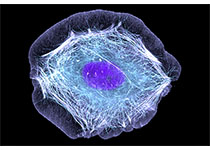
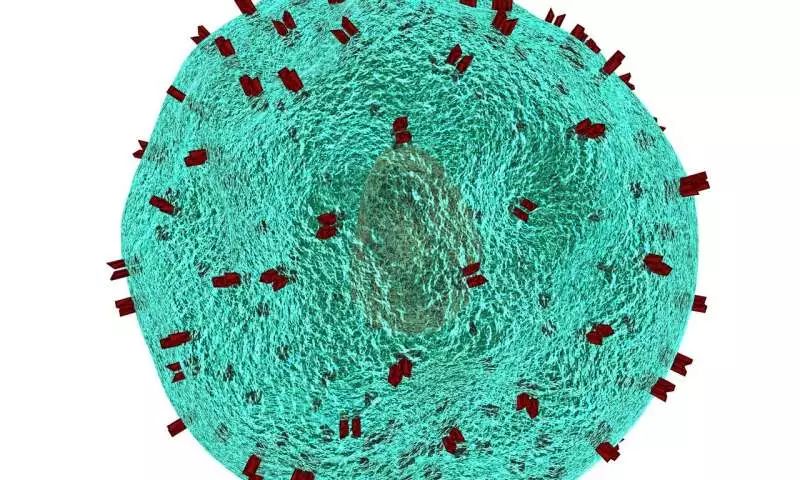
Plos Biology:利用人干细胞“年轻因子”治疗骨关节炎取得新进展
2019-04-23 刘光慧研究组 中科院生物物理所
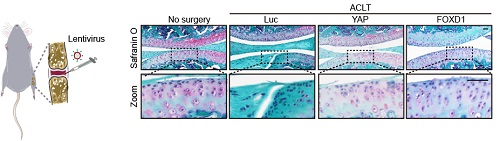
近期,中科院生物物理所刘光慧研究组同北京大学汤富酬研究组、中科院动物所曲静研究组合作,在PLOS Biology在线发表题为“Up-regulation of FOXD1 by YAP alleviates senescence and osteoarthritis”的研究论文。该研究首次报道了YAP-FOXD1通路在人干细胞去衰老(De-senescence)及骨关节炎基因治疗中的作用及分子机制
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#骨关节#
66
#Bio#
74
#Biol#
62
学习了噢。。
104
#关节炎#
64
学习
97
学习啦。。。
109