BMJ:静止期溃疡性结肠炎患者并发肠外溃疡
2019-04-11 不详 消化界
2019年3月28日,英国圣赫利尔医院的Tewari A教授等在The BMJ上,报道了1例静止期溃疡性结肠炎(UC)患者出现皮肤多发性溃疡病例,并发的溃疡与UC的相关性以及如何治疗?
基本病史
患者男性,65岁,患有UC,1周前下肢、会阴和造口周围皮肤出现坏死性溃疡,病情进展快速,伴有疼痛。无肠道症状。18个月前,患者接受了次结肠切除术和造口术,UC症状有所缓解,此后一直没有治疗。
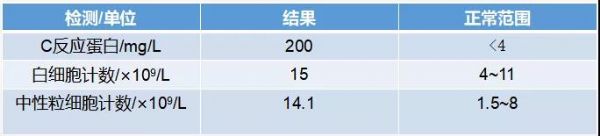
在体格检查过程中,患者发热、嗜睡,格拉斯哥昏迷量表评分为14/15。患者造口功能良好。双下肢大面积区域以及右侧腹股沟10cm×5cm区域有多个中凹型溃疡,边缘呈紫色。整个造口外周也并发溃疡。血液结果如表1所示。

图1 双下肢广泛溃疡,边缘凸起
表1 血液检测结果
所有伤口拭子和血培养均为阴性。
问题
1.诊断是什么?
2.这种情况与炎症性肠病之间有什么联系?
3.这种情况有哪些治疗方案?
1
诊断是什么?
坏疽性脓皮病是一种较为罕见的皮肤溃疡性疾病。在炎症性肠病中,坏疽性脓皮病通常与结肠炎活动度有关,但少数情况下结肠炎静止期亦可存在。
患者有UC疾病基础,并发了快速进展的疼痛性溃疡,符合溃疡型坏疽性脓皮病和造口周围的坏疽性脓皮病。坏疽性脓皮病通常以小丘疹开始发病并迅速进展,且经常被误诊为感染或血管炎。伤口培养检测最初往往呈阴性,但是在皮肤破裂后,伤口会发生继发感染。
由于潜在的全身性疾病,或是坏疽性脓皮病相关的炎症,可能导致炎症标志物升高。坏疽性脓皮病在高达50%的病例中是特发性的,但可能与UC、骨髓增生异常、淋巴瘤、关节炎和某些药物有关。框1中显示了不同的坏疽性脓皮病。
方框1:坏疽性脓皮病类型及其表现
溃疡型坏疽性脓皮病
溃疡迅速发展,边缘呈典型的紫罗兰色。是最常见但也是最严重的类型;
脓疱型坏疽性脓皮病
离散性脓疱,周围有红斑晕,通常与炎症性肠病有关;
大疱型坏疽性脓皮病
分组的囊泡聚结形成大的大疱。通常与骨髓增生异常有关;
植物型坏疽性脓皮病
呈现为红斑性溃疡斑块,没有特征性破坏边界。可能会发展为糜烂;
造口周围坏疽性脓皮病
由于创伤和过敏反应,可能发生在造口部位周围。发病时间从造口形成后的两周到三年内。
2
这种情况与炎症性肠病之间有什么联系?
大约30%~60%的坏疽性脓皮病与UC有关。同时,大约2%~8.5%的UC患者可能会发生坏疽性脓皮病,这种情况在CD患者中不太常见。
无论肠道状态如何,UC患者的细胞因子谱是一种危险因素,并且在全或次结肠切除术后以及无UC症状时都有可能发生坏疽性脓皮病。有些坏疽性脓皮病在经过结肠切除术后有所改善,因此最初该病的发病机制被认为与肠道疾病活动有关。推测UC中性粒细胞功能紊乱导致炎症反应和IL1β、TNFα、IL6、IL8、IL17、IL23等的流入,以及基质金属蛋白酶的产生,其可能在坏疽性脓皮病的发病中起作用。另外,在坏疽性脓皮病组织学样品中也可以检测到这些细胞因子。
尽管进行了肠或直肠切除术,进展性坏疽性脓皮病和其他UC肠外临床表现的遗传易感性仍然存在,甚至在没有UC症状的情况下也是如此。
3
这种情况有哪些治疗方案?
高剂量类固醇(静脉注射、口服)和(或)免疫抑制剂。
抗生素(如米诺环素、强力霉素)的抗炎作用可以帮助减少细胞因子流入并抑制中性粒细胞功能,以及抗菌特性。氨苯砜(一种抗炎和抗微生物复合物)同样有用。
超强效类固醇可用于局部疾病。大多数患者需要全身治疗,如糖皮质激素,其可以诱导快速反应。其他治疗选择包括环孢素、硫唑嘌呤、甲氨蝶呤和霉酚酸酯(较少的肝毒性)。另外,抗肿瘤坏死因子抑制剂如英夫利西单抗和阿达木单抗在治疗中的效果也已得到充分验证。而IL1受体拮抗剂是一种新兴疗法。
尽管进行了UC肠/直肠切除术,但是坏疽性脓皮病的易感性仍然存在。
学习要点
?溃疡型坏疽性脓皮病溃疡进展快速,边缘呈典型的紫罗兰色;
?溃疡型坏疽性脓皮病是最常见的坏疽性脓皮病(PG)类型,可能是最严重的类型;
?30%~60%的溃疡型坏疽性脓皮病病例与UC相关联;
?造口周围坏疽性脓皮病的发作可发生于造口形成后2周至3年。
患者预后
坏疽性脓皮病作为溃疡性结肠炎的肠外表现之一,需要临床医师早期发现,充分认识,给予患者个体化治疗,及早控制病情,改善预后。
原始出处:
Tewari A, Mahmood A et,al. Multiple eruptive ulcers in a patient with quiescent ulcerative colitis. BMJ. 2019 Mar 28;364:l847. doi: 10.1136/bmj.l847.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#并发#
61
#溃疡性#
65
#肠外溃疡#
0
#BMJ#
59