BMJ:丹麦和挪威的牛津-阿斯利康ChAdOx1-S疫苗接种后的动脉事件、静脉血栓栓塞、血小板减少和出血
2021-05-06 MedSci原创 MedSci原创
ChAdOx1-S疫苗接种后栓塞(包括脑静脉血栓形成)的发生率高于正常水平。这些事件的绝对风险很小。对于其余的安全结果,结果令人放心,血小板减少/凝血障碍和出血的发生率略高,这可能受到加强监测的影响。
截至2021年4月初,新冠肺炎大流行已影响全球13亿多人,280万人死亡;疫苗是控制大流行最有力的工具;目前,欧盟批准了四种疫苗用于covid-19,分别是辉瑞生物科技公司(Comirnaty)、 Moderna、牛津-阿斯利康公司(Vaxzevria)、和最近的janssen公司。在大型随机对照试验中,这些疫苗对有症状的covid-19的疗效已达到66%至95%。
丹麦和挪威科学中心目前合作的研究的目的是评估ChAdOx1-S疫苗接种后28天内心血管和出血事件的发生率,并将这些发生率与两国普通人口中相应的年龄和性别标准化率进行比较。

纳入2021年2月9日至2021年3月11日期间接种ChAdOx1-S首剂疫苗的18-65岁人群。丹麦(2016-18)和挪威(2018-19)的一般人群作为比较队列。测量观察了28天内接种人群中因动脉事件、静脉血栓栓塞、血小板减少/凝血障碍和出血而住院接触的发生率,并与预期的发生率进行了比较,这是基于两国普通人群中特定年龄和性别背景的发生率。
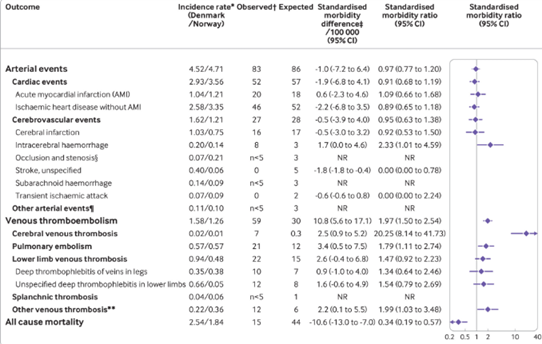
接种疫苗的队列包括丹麦的148792人(中位年龄45岁,80%为女性)和挪威的132472人(中位年龄44岁,78%为女性),他们接受了第一剂ChAdOx1-S。在281264名ChAdOx1-S接种者中,动脉事件的标准化发病率为0.97(95%可信区间0.77 - 1.20)。

在接种队列中观察到59例静脉血栓栓塞事件,而根据一般人群的发病率预计为30例,对应的标准化发病率为每10万疫苗接种1.97(1.50至2.54)和11(5.6至17.0)的额外事件。脑静脉血栓形成率高于预期:标准化发病率为20.25 (8.14 ~ 41.73);每100 000次疫苗接种超过2.5(0.9至5.2)次。任何血小板减少/凝血障碍的标准化发病率比率为1.52(0.97至2.25),任何出血的标准化发病率比率为1.23(0.97至1.55)。在疫苗队列中观察到15例死亡,而预期为44例。

在牛津-阿斯利康covid - 19疫苗(ChAdOx1-S) 18-65岁患者的大型两国队列研究中,结果显示,大多数心血管和止血结果可靠。然而,确实观察到静脉血栓栓塞事件发生率的增加,在282 572名疫苗接种者中,有7个观察到的脑静脉血栓形成发生率明显高于0.3个预期的发生率(超过每10万名疫苗接种者中的2.5个,或每4万名疫苗接种者中的1个)。相反,没有观察到整体动脉事件率的增加。观察到血小板减少/凝血障碍和出血的发生率略有增加,但是,在分析中排除短暂的医院接触(<5小时)后,该发生率减弱。
该研究发现ChAdOx1-S疫苗接种后栓塞(包括脑静脉血栓形成)的发生率高于正常水平。然而,这些事件的绝对风险很小。对于其余的安全结果,结果令人放心,血小板减少/凝血障碍和出血的发生率略高,这可能受到加强监测的影响。鉴于covid-19疫苗接种已被证实的益处,以及全球严重SARS-CoV-2感染病例的高发病率,这项研究中描述的绝对风险很小。
原文出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ChAdOx1#
81
#静脉#
59
#BMJ#
48
#静脉血#
58
阅读阅读阅读
70
#疫苗接种#
42
#血小板减少#
54