2019 ASCO:诺华和默克治疗MET突变非小细胞肺癌的候选药,在2期临床均显示出治疗活性
2019-06-04 不详 MedSci原创
在美国ASCO大会上,诺华和默克都报告了用于治疗MET突变非小细胞肺癌(NSCLC)药物的2期临床试验结果。
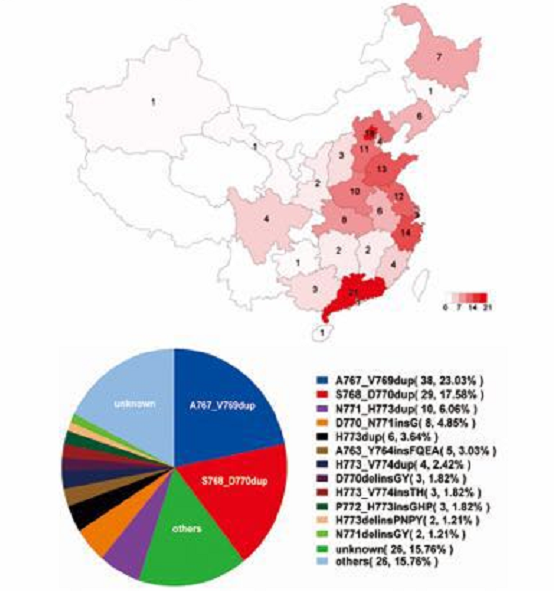
诺华的capmatinib和默克的tepotinib均靶向MET信号通路,有3%~5%的NSCLC患者发生MET突变,该突变并且往往会引起预后不良的侵袭性肿瘤。
诺华的capmatinib在2期GEOMETRY mono-1试验中的结果显示,58名先前未接受过治疗的患者总体反应率为68%,69名先前接受过治疗的患者总体反应率为41%,中位反应持续时间分别为11.1和9.7个月。
还有证据表明,capmatinib能够治疗转移到大脑的癌变,该类别13名患者中有7名表现出反应并且"包括一些完全消除脑部病变的病例"。
默克的tepotinib在2期tepotinib研究结果显示,57例患者中通过MET血液学检测显示有50%达到客观反应,58例通过组织活检确定的患者中有45%达到客观反应,中位反应持续时间为12至17个月。Tepotinib似乎也适用于脑转移患者,患者从治疗中"同样受益"。
在这个阶段,两种药物之间的直接比较是困难的,但令人鼓舞的是,两者似乎都在患者组中具有活性,而这类患者目前没有针对性的治疗选择,通常用铂化疗。
原始出处:
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#非小细胞#
56
#MET#
53
#2期临床#
57
#默克#
52
#诺华#
52
#ASC#
0