NEJM:警惕胸腔穿刺术后复张性肺水肿并发症
2014-08-01 MedSci MedSci原创
患者,男,67岁,患有晚期酒精性肝硬化,因渐进性呼吸困难入院治疗。胸片显示右侧胸腔有大量积液(A图)。因怀疑为肝性胸水,对其进行 胸腔穿刺术,抽取渗出液1500ml。 A图 4小时后出现咳嗽、呼吸急促、心动过速症状,听诊右肺湿罗音。氧饱和度为82%。胸部CT显示右肺散在实变影及磨玻璃样阴影(B图),表明为复张性肺水肿。 B图 患者接受利尿剂治疗及
患者,男,67岁,患有晚期酒精性肝硬化,因渐进性呼吸困难入院治疗。
胸片显示右侧胸腔有大量积液(A图)。因怀疑为肝性胸水,对其进行 胸腔穿刺术,抽取渗出液1500ml。

A图
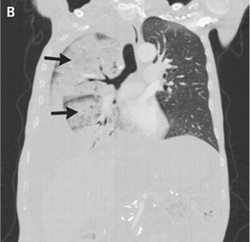
B图

C图
原始出处:
Perricone G, Mazzarelli C.Images in clinical medicine. Reexpansion pulmonary edema after thoracentesis.N Engl J Med. 2014 Mar 20;370(12):e19. doi: 10.1056/NEJMicm1309844.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








和普通大量胸腔积液行胸腔闭式引流一样,肯定有规定,一次引流量和速度有控制,不然会引起复张性肺水肿。
104
好东西
119
好东西,学习一下
111
#胸腔穿刺术#
99
#并发#
86
#穿刺#
92
#水肿#
80