Communnications Biololgy:卵巢癌早筛难?液体活检来支援—新型血浆蛋白标记物
2019-07-04 佚名 转化医学网
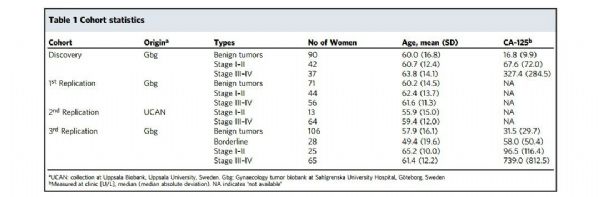
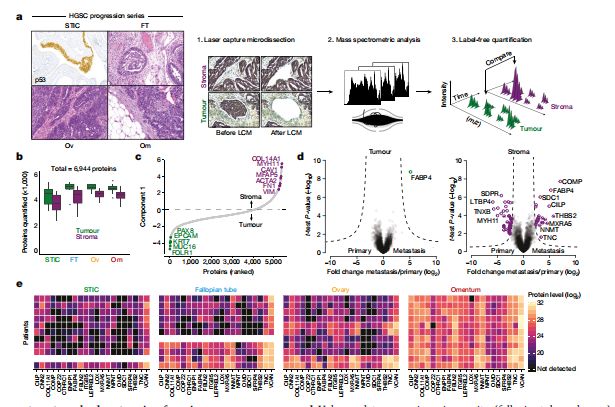
近日,来自乌普萨拉大学和哥德堡大学Sahlgrenska学院的科学家表示,他们已经开发了一种血液检测方法,通过高通量蛋白质组学确定了卵巢癌的11种高精确度的血浆蛋白生物标志物,可以为疑似卵巢癌提供更准确的诊断,有望为卵巢癌高危患者提供早期筛查,降低了卵巢癌患者的剖腹探查术的手术率。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#标记物#
36
#血浆蛋白#
37
#Bio#
41
#Biol#
36
#活检#
36
#早筛#
30
#COMMUN#
40