盘点:肾癌近期重要研究进展一览
2017-09-16 MedSci MedSci原创
肾细胞癌(Renal Cell Carcinoma, RCC)是最常见的泌尿器恶性肿瘤之一,来源于肾上皮组织,占肾恶性肿瘤的85%左右,流行病学研究表明其发病仍处上升趋势。25%的RCC患者初诊时已出现周围组织侵犯和/或远处转移。并且30%诊断为局限性疾病且接受根治手术的患者,术后很快发生局部复发或远处转移,5年生存率小于10%。这里梅斯小编整理了近期关于肾癌的重要研究进展与大家一同分享。【1
肾细胞癌(Renal Cell Carcinoma, RCC)是最常见的泌尿器恶性肿瘤之一,来源于肾上皮组织,占肾恶性肿瘤的85%左右,流行病学研究表明其发病仍处上升趋势。25%的RCC患者初诊时已出现周围组织侵犯和/或远处转移。并且30%诊断为局限性疾病且接受根治手术的患者,术后很快发生局部复发或远处转移,5年生存率小于10%。这里梅斯小编整理了近期关于肾癌的重要研究进展与大家一同分享。
【1】沃利替尼治疗晚期肾癌Ⅱ 期临床试验结果喜人
沃利替尼(Savolitnib)是一种新型的选择性的MET基因抑制剂,在先期的Ⅰ期临床试验中在MET驱动型的PRCC中显现出了良好的抗肿瘤活性,其治疗晚期乳头状肾癌的全球、多中心、单臂的Ⅱ期临床试验(Clinicaltirals.gov ID:NCT02127710)结果在2017 ASCO GU上做了汇报。结果显示,沃利替尼(Savolitnib)可有效抑制MET驱动型PRCC患者的肿瘤进展,ORR达到18%,临床获益率达68%。MET驱动型的中位PFS也明显高于MET非依赖型(6.2个月 vs 1.4个月)。该Ⅱ期研究显示,沃利替尼在MET驱动型PRCC患者中表现出了较好的抗肿瘤的活性及安全性,后续Ⅲ期临床结果令人期待。
【2】世上首个肾癌模型建成
经过长期的科研攻坚,苏黎世大学Ian Frew教授实验室的科学家们终于开发出了可用于研究肾细胞癌的老鼠模型。研究人员首先鉴定了人类肾细胞癌中的常见突变基因,然后他们同时突变了小鼠肾细胞中的其中3个基因,从而成功构建了肾癌动物模型。这种疾病模型的重现,将为更好的肾癌治疗手段开发提供思路。使用与人类相同的药物,研究人员也可在小鼠模型中观察这些现象。小鼠模型也有助于免疫疗法的进一步发展。这项技术在过去几年中已经取得了很大的进步。如今,新模型的问世,将使科学家们可以在正常的体内免疫系统环境下研究肾肿瘤的发育,以及癌细胞逃避免疫系统攻击的原理。最终,科学家们的目标是利用这些新发现来提高免疫调节治疗的效果。
【3】针对晚期肾癌的靶向药物表现出治疗新希望
根据Dana-Farber癌症研究所的研究显示,一些具有预后不良的晚期肾癌患者受益于针对导致癌性生长的异常遗传途径的实验药物。该药物savolitinib在转移性乳头状肾细胞癌(PRCC)患者中表现出临床活性,其肿瘤由MET信号通路的过度活动驱动,但对于肿瘤缺乏MET异常的患者无效。目前的试验测试了109例局部晚期或转移性PRCC患者的savolitinib使用情况。在109例患者中,40%患有MET驱动的肿瘤,42%患有不依赖MET的肿瘤,17%的患者的MET状态未知。当分析结果时,18%的MET驱动癌症患者肿瘤明显收缩,50%患者疾病稳定。相比之下,MET独立型肿瘤患者均没有收缩反应,只有24%的患者病情稳定。此外,在MET驱动的肿瘤组中,肿瘤开始生长之前的治疗时间长度显着延长 - 6.2个月至1.4个月。
【4】肾癌的免疫组合治疗或成为治疗新标准
近期,一项来自德州大学西南医学中心的临床试验宣布,用ipilimumab(Yervoy)和nivolumab (Opdivo, 纳武单抗)两种抗体药物组合治疗肾癌,可以将癌症缓解率提高到前所未有的40%,比之前整整多了一倍!经典的化疗对肾癌的治疗效果一直不太理想。靶向治疗虽然可以延长患者的生命,但也带来一些副作用。单个药物的免疫治疗可以提高患者的生存率,但也只对一部分患者有效。所以在肾癌治疗领域,还有很大的医疗需求未被满足。该免疫组合治疗涉及的两种药物——ipilimumab和nivolumab (纳武单抗),都已经通过美国FDA批准上市,如果后面的试验结果依旧良好,这种方法将会成为新的肾癌标准治疗方案。
【5】IL-6R抑制剂和TKI的联合治疗或能为肾癌治疗提供一种新型治疗方法
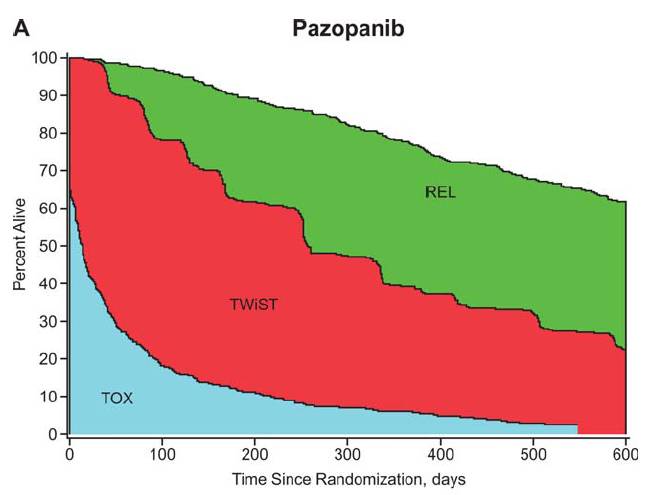
肾癌治疗护理中,TKI代表一定的参考标准,然而相当一部分RCC患者会对这种治疗产生耐药性。白细胞介素-6(IL-6)被认为与RCC的预后不良相关,研究人员推测TKI抗性和IL-6分泌有着一定的因果联系。结果显示,786-O RCC细胞在TKIs sorafenib、sunitinib 和pazopanib低剂量刺激后表现出IL-6的高水平分泌,诱导AKT-mTOR通路的激活以及NFκB、HIF-2α和VEGF的表达。小鼠异种移植模型显示,tocilizumab与低剂量sorafenib联合治疗抑制786-O肿瘤生长、抑制AKT-mTOR通路,并且在抑制体内血管生成作用方面比单用sorafenib更有效。表明IL-6R抑制剂和TKI的联合治疗或能为RCC治疗提供一种新型治疗方法。
【6】两个主要的来源的肾癌细胞系分析可成功进行基于基因组的细胞系选择
癌细胞系的利用可以被相似性的内源性肿瘤细胞影响。最近,有研究人员将来自癌症细胞系百科和COSMIC细胞系工程的来源于肾的65个细胞系的基因组数据与来源于肿瘤基因组计划的3种肾癌细胞亚型进行了比较,这3中肾细胞亚型分别为:肾透明细胞癌(ccRCC),肾乳头状细胞癌(pRCC)和肾难染性细胞癌(chRCC)。研究发现,聚类拷贝数改变表明了大多数细胞系类似于ccRCC,有一些细胞系类似于pRCC,但是没有细胞系类似于chRCC。人类ccRCC肿瘤与细胞系聚类表现了更加具有侵入性疾病的临床和基因组特性,表明了细胞系能够最好的代表侵入性肿瘤。研究人员通过数据库之间的一致性,分层分析了重要肾癌基因的突变和拷贝数改变,并且将细胞系基于基因表达分类为懒惰性亚型和侵入性亚型。最后,研究人员指出,这些结果可以帮助研究者分析合适的肾癌细胞系。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











学习了谢谢分享!!
107
#研究进展#
0
学习了.谢谢分享
100
谢谢分享.继续关注
88
感谢小编为我们准备了如此丰盛的精神大餐.同时也向作者致谢!认真学习了.点赞!
82
学习了谢谢分享
81