中间型链球菌感染性鼻窦炎导致急性硬膜下脓肿1’例
2019-09-12 杜安东 别鹏飞 许世辉 中国微侵袭神经外科杂志
男,13岁。因发热、头痛伴呕吐3d入院。入院3d前因发热、头痛于本院儿科就诊,考虑呼吸道感染予以对症治疗后,症状无缓解且出现恶心呕吐,再次就诊。行头部CT扫描(图1A、1B)提示右侧额颞顶硬膜下积液,颅内积气,环池及右侧脑室受压,中线结构轻度移位,副鼻窦炎。既往慢性鼻窦炎病史5年,无头部外伤史,入院查体无明显神经系统阳性体征。
鼻窦炎导致颅内感染形成硬膜下脓肿的病例极为罕见,临床诊断及治疗较困难,一旦漏诊、误诊失去最佳治疗时间、方式,可能危及病人生命或遗留严重并发症。宁夏回族自治区人民医院神经外科2018年收治1例中间型链球菌感染性鼻窦炎致颅内感染病人,并复习相关文献以提高对该病的诊治能力,现报告如下。
1.病历摘要
男,13岁。因发热、头痛伴呕吐3d入院。入院3d前因发热、头痛于本院儿科就诊,考虑呼吸道感染予以对症治疗后,症状无缓解且出现恶心呕吐,再次就诊。行头部CT扫描(图1A、1B)提示右侧额颞顶硬膜下积液,颅内积气,环池及右侧脑室受压,中线结构轻度移位,副鼻窦炎。既往慢性鼻窦炎病史5年,无头部外伤史,入院查体无明显神经系统阳性体征。
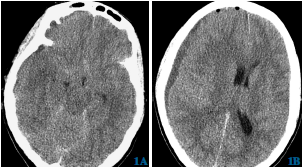
图1A、1B术前头部CT示环池受压消失、右侧硬膜下脓肿
血常规检查:白细胞17.77×109/L,中性粒细胞百分比86.6%,降钙素原测定72.21ng/ml,暂给予抗感染、脱水降颅内压、止吐等对症治疗。入院8h后,病人意识障碍程度加重,神志呈浅昏迷,右侧瞳孔散大,直径4.0mm,光反射消失,考虑脑疝形成。
复查头部CT示:右侧额颞顶硬膜下积液量较前略微增加,脑肿胀加重,中线结构移位加剧,环池及右侧脑室受压明显。立即送往手术室拟行去骨瓣减压术,术中于右顶结节钻孔,刺破硬脑膜可见乳白色脓液流出,留取标本行细菌培养加药物敏感试验,待大部分脓液排出后,给予医用双氧水、庆大霉素盐水(800U/ml)反复冲洗脓腔,直至冲洗液清亮后,硬膜下置管持续引流。
术后病人瞳孔恢复正常,清醒后返回病房监护治疗,术后头部CT扫描(1C、1D),术后考虑急性硬膜下脓肿,初期给予头孢曲松钠(2g/次,2次/d)静脉滴注并庆大霉素8万U及生理盐水通过引流管冲洗硬膜下脓腔1次/d。术后第3天病人出现高热并癫痫发作,给予丙戊酸钠静脉抗癫痫治疗。术中标本培养结果回报:中间型链球菌感染,根据药敏结果调整抗生素为万古霉素500mg/次,4次/d。
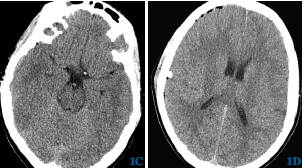
图1C、1D硬膜下钻孔引流术后头部CT示环池显影、右侧硬膜下脓肿消失
完善副鼻窦CT(图1E)、头部MRI(图1F、1G)检查,考虑感染来源于副鼻窦。经治疗10d后病人体温恢复正常,癫痫得到控制,血常规、降钙素原测定、超敏C反应蛋白恢复正常。耳鼻喉医师会诊后建议行鼻内镜下脓肿引流术,家属考虑病人年龄较小,希望药物保守治疗,糠酸莫米松50μg/(次·d)涂鼻腔,克拉霉素0.75g/(次·d)。病人未做鼻窦炎手术,颅内病情平稳后出院。1个月后复查副鼻窦炎消失,3个月后电话随访病人无鼻窦炎症状,无癫痫发作。
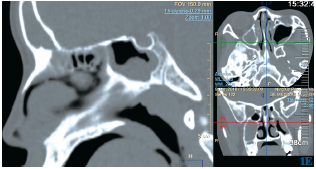
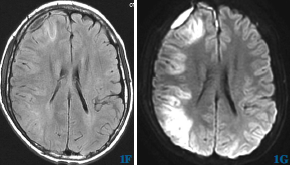
图1E术后鼻窦CT示额窦、筛窦、蝶窦、上颌窦均见等密度脓肿影1F、1G术后头部MRI示残存脓肿
2.讨论
随着抗生素治疗在临床上的广泛使用,细菌导致颅内感染的并发症日益罕见,大部分经保守治疗可治愈,但极少部分仍需要外科手术治疗。免疫功能正常的病人,急慢性鼻窦炎导致颅内感染是一种相对罕见的临床病例,而由中间型链球菌连续传播引起的额叶急性硬膜下脓肿国内尚无报道。查阅文献约有3%的急性鼻窦炎病人会进展为颅内并发症,主要包括硬脑膜外脓肿、硬脑膜下脓肿、化脓性脑膜炎、脑脓肿、海绵窦血栓性静脉炎。更有鼻窦炎引起脑内脓肿致非交通性脑积水最终造成病人死亡的报道。
急性鼻窦炎合并颅内感染临床工作中少见,容易误诊、漏诊。但一旦诊断明确后应积极抗感染治疗,抗炎24~48h治疗无效,复查脓肿范围较前增加,可在鼻内镜下行副鼻窦内脓肿引流术以避免更严重的并发症,而对于颅内并发症严重者可行手术清除颅内感染灶。
本例病人2次就诊儿科门诊,初次误诊为上呼吸道感染,因发热伴恶心、呕吐症状加重再次就诊,行头部CT检查明确颅内病变后收住神经外科。入院后8h出现意识障碍加重并脑疝形成,急诊行硬膜下钻孔引流术,术后病人瞳孔、意识恢复正常。术中证实硬膜下积脓,术后细菌培养证实系中间型链球菌感染,结合病史,考虑原发病为鼻窦炎。
中间型链球菌为一组链球菌(Str.intermedius group),包括3个菌种:中间型链球菌(Str.intermedius)、星座链球菌(Str.contellatus)和咽峡链球菌(Str.anginosus),首次由GUTHOF在1956年报道,源于口腔脓肿。该组细菌主要存在于人类口腔,也可存在于咽喉及胃肠道,可致牙龈脓肿、吸入性肺炎,并可由此引起败血症、心内膜炎、肺脓肿和脓胸,也有文献报道该组链球菌可引起脑脓肿,并常与厌氧菌同时存在。与其他病原体相比,中间型链球菌感染往往需要更积极的外科手术干预和较长疗程的抗生素治疗。
β-内酰胺类抗生素常有效,头孢曲松是治疗的热门选择。而病情的转归往往取决于病人的免疫状态、感染、创伤或治疗史,一旦延误可能造成难以挽回的结果。本组治疗初期未检测原发灶细菌,依据术中病情选用抗菌谱较广又易通过血-脑屏障的庆大霉素和具有强氧化能力、能破坏细菌菌体、杀死细菌的双氧水,同时冲洗脓腔。术后病人出现癫痫发作是病情进展导致还是与治疗过程中药物冲洗脓腔刺激大脑皮质导致,尚不能明确,有待进一步研究,本组的治疗经验仅供参考。
脑脓肿往往通过早期脑炎进展到包膜形成期,包膜形成包括新生血管、成纤维细胞和神经胶质细胞的积累,通常会导致癫痫发作,并长期留有后遗症。鼻腔和副鼻窦慢性炎症是颅内感染的高危因素。那么鼻窦炎如何导致急性硬膜下脓肿的呢?查阅文献主要有以下3种途径:①直接侵犯颅前底骨质,造成骨髓炎进而累及颅内。②经颅底先天及后天形成的缺损侵及颅内。③经颅前底无静脉瓣的板障静脉累及颅内。
综上所述,作者认为:病人长期鼻窦炎病史,累及颅前底骨质,鼻腔及副鼻窦黏膜水肿使得腔内压力骤升,突破薄弱骨质致鼻窦内脓液进入颅内,导致硬膜下积脓,同时使颅内与外界短暂开放,导致颅内积气。鼻源性颅内感染是由邻近副鼻窦化脓性感染侵入颅内所致,如额窦炎、筛窦炎、上颌窦炎或蝶窦炎,感染灶通过颅底导血管蔓延至颅内,多在额叶前部或底部形成脓肿。而血行播散性病例往往是多发的,出现在大脑中动脉区域,常位于灰质白质界面。
临床上急性硬膜下脓肿、慢性硬膜下血肿、慢性硬膜下积液CT均表现为硬膜间隙增宽,难以鉴别,头部MRI有助于诊断。因此,作者认为对于无头部外伤史而怀疑急性硬膜下脓肿的病人应接受急诊MRI检查,以排除急性硬膜下脓肿的可能。然而大多数病人很难及时行此项检查,主要在于临床医师对疾病的认识不够和MRI检查的普及不足。本病的预后取决于是否及时诊断、治疗、入院时病情的严重程度和意识障碍程度,以及术后并发症的预防和治疗。值得一提的是,实验室检查也尤为重要,如C-反应蛋白、降钙素原测定和红细胞沉降率有助于确定是否存在感染,其可以指导治疗。
原始出处:
杜安东,别鹏飞,许世辉,李敏,高阳,兰彦平,兰茂升,张吉云,李永财.中间型链球菌感染性鼻窦炎导致急性硬膜下脓肿并相关文献复习[J].中国微侵袭神经外科杂志,2018(07):320-322.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#感染性#
105
#硬膜下#
86
#脓肿#
81
#链球菌#
81