Transgelin 先天性心脏病相关的肺动脉高压患者的肺动脉平滑肌细胞功能障碍
2022-07-20 刘少飞 MedSci原创
Transgelin 是一种肌动蛋白结合蛋白,可调节肺动脉平滑肌细胞 (PASMC) 功能障碍。本研究旨在探讨transgelin在CHD-PAH发病机制中的分子机制和生物学功能。
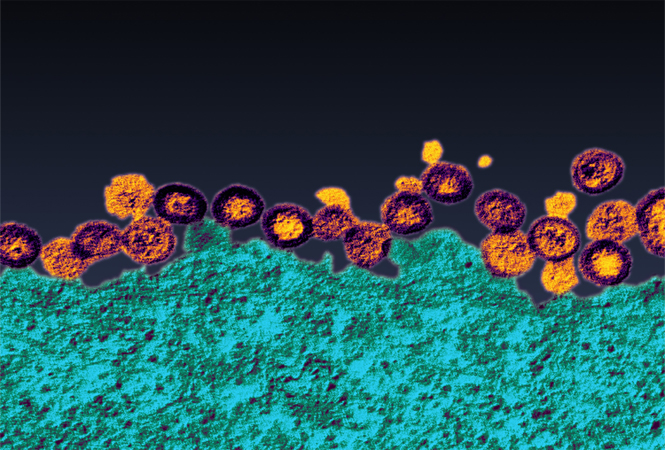
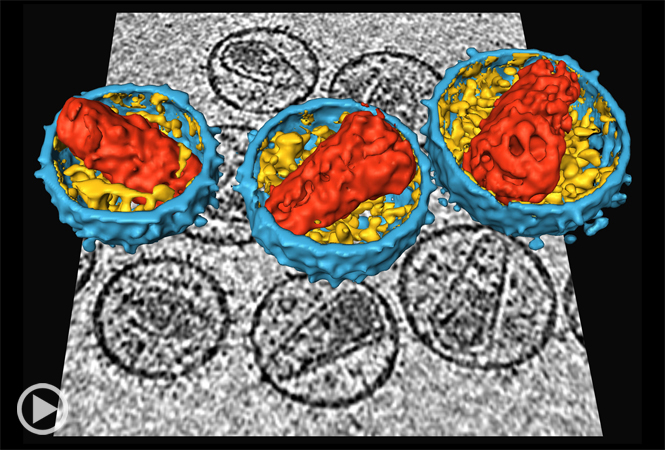
肺动脉高压(PAH)是先天性心脏病(CHD)较为常见的并发症。其特征是由于异常的细胞增殖、纤维化和原位血栓形成导致小肺动脉进行性变窄,最终导致肺血管阻力连续升高和随后的右心室衰竭。协调从可逆的内侧肥大到不可逆的丛状病变的转变对于先天性心脏病相关的肺动脉高压 (CHD-PAH) 至关重要。Transgelin 是一种肌动蛋白结合蛋白,可调节肺动脉平滑肌细胞 (PASMC) 功能障碍。本研究旨在探讨transgelin在CHD-PAH发病机制中的分子机制和生物学功能。
研究方法和结果:
通过免疫组织化学在 CHD-PAH 患者和野百合碱 (MCT) 加主动脉腔静脉 (AV) 诱导的 PAH 大鼠的肺组织中检测到 Transgelin 表达。在体外,分别通过细胞计数和 EdU 测定、transwell 迁移测定和 TUNEL 测定评估了 transgelin 对人 PASMC (HPASMC) 增殖、迁移和凋亡的影响。并通过免疫印迹法评估转凝胶蛋白对 HPASMC 表型标志物表达的影响。(i) 与正常对照组 (n = 12) 相比,transgelin 表达在可逆 (n = 15) 和不可逆 CHD-PAH 组 (n = 4) 的肺小动脉中显着过表达(可逆组与对照组) :18.2 ± 5.1 vs. 13.6 ± 2.6%,P < 0.05;不可逆组 vs. 对照组:29.9 ± 4.7 vs. 13.6 ± 2.6%,P < 0.001;不可逆组与可逆组:29.9 ± 4.7 vs. 18.2 ± 5.1,P < 0.001)。这一结果在 MCT-AV 诱导的 PAH 大鼠中得到进一步证实。此外,transgelin表达水平与CHD-PAH患者肺动脉病理分级呈正相关(r = 0.48,P = 0.03,n = 19)。(ii) 与正常对照组 (n = 12) 相比,TGF-β1 表达在可逆 (n = 15) 和不可逆 CHD-PAH 组 (n = 4) 的肺小动脉中显着过表达(可逆组 vs.对照组:14.8 ± 4.4 vs. 6.0 ± 2.5%,P < 0.001;不可逆组 vs. 对照组:20.1 ± 4.4 vs. 6.0 ± 2.5%,P < 0.001;不可逆组 vs. 可逆组:20.1 ± 4.4 vs. 14.8 ± 4.4,P < 0.01)。在 CHD-PAH 患者 (r = 0.48, P = 0.04, n = 19) 和 MCT-AV 诱导的 PAH 大鼠中证实了 TGF-β1 和 transgelin 之间的进展依赖性相关性,这在亚细胞水平上得到了进一步证实。(iii) transgelin 的敲低通过抑制 TGF-β1 信号通路减少了 HPASMCs 的增殖、迁移、凋亡抗性和表型转化。相反,transgelin 过度表达导致相反的效果。

研究结论:
这些结果表明,transgelin 可能通过正向调节 TGF-β1 信号通路促进 HPASMC 功能障碍,成为 CHD-PAH 发展的指标,也是治疗 CHD-PAH 的潜在治疗靶点。
参考文献:
Zhou JJ, Yang J, Li L, Quan RL, Chen XX, Qian YL, Huang L, Wang PH, Li Y, Meng XM, Chen X, Gu Q, He JG. Transgelin exacerbates pulmonary artery smooth muscle cell dysfunction in shunt-related pulmonary arterial hypertension. ESC Heart Fail. 2022 Jul 15. doi: 10.1002/ehf2.14080. Epub ahead of print. PMID: 35841124.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#动脉高压#
77
#平滑肌#
67
#TRA#
73
#肺动脉高压患者#
76
#平滑肌细胞#
76
#先天性#
59
#功能障碍#
82
#细胞功能#
56