高频超声诊断女性婴幼儿腹股沟附件嵌顿疝2例
2019-10-25 宋建 张文君 雷琳 中国临床医学影像杂志
例1,女,3岁,因发现右侧腹股沟包块4天入院。查体:右侧腹股沟区见大小约1.5 cm×1.5 cm包块,伴触痛,不可还纳入腹腔。超声检查:右侧腹股沟区探及范围约3.6 cm×1.5 cm疝囊,内见大小约2.4 cm×1.4 cm实性回声团(图1),向下追踪,其与腹腔内一囊实性结构相连(图2),CDFI于该结构内探及血流信号,近端显示血流来源于髂内动脉。超声提示:右侧腹股沟疝(疝内容物为右侧输卵管可
例1,女,3岁,因发现右侧腹股沟包块4天入院。查体:右侧腹股沟区见大小约1.5 cm×1.5 cm包块,伴触痛,不可还纳入腹腔。超声检查:右侧腹股沟区探及范围约3.6 cm×1.5 cm疝囊,内见大小约2.4 cm×1.4 cm实性回声团(图1),向下追踪,其与腹腔内一囊实性结构相连(图2),CDFI于该结构内探及血流信号,近端显示血流来源于髂内动脉。超声提示:右侧腹股沟疝(疝内容物为右侧输卵管可能)。

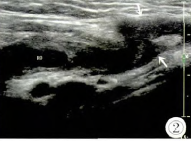
图1 疝内容物为右侧输卵管声像图(ROD:右侧输卵管,箭头:疝囊)。图2 右侧卵巢声像图(RO:右侧卵巢,箭头:疝囊)。
例2,女,1月23天,因发现右侧腹股沟包块1天入院。查体:右侧腹股沟区见大小约3.0 cm×2.5 cm包块,局部红肿,触诊包块张力较高,不能还纳。超声检查:右侧腹股沟区见一范围约2.4 cm×1.7 cm椭圆形混合回声团块,实时观察未见蠕动,内可见多个大小不等无回声区(图3)。CDFI显示上述团块周边及内部未见明显血流信号(图4)。超声提示:右侧腹股沟嵌顿疝(疝内容物为卵巢可能)。

图3 疝内容物为右侧卵巢声像图(箭头:腹壁缺损)。图4 疝内容物为右侧卵巢CDFI图。
行腹腔镜探查术:右侧内环口见一卵巢嵌顿,大小约2.5 cm×2.0 cm,呈黑紫色,子宫及右侧输卵管明显向右侧内环口移位,右侧输卵管明显充血、水肿,左侧内环口无明显裂隙。术中确诊:右侧腹股沟斜疝并卵巢嵌顿。考虑到患儿年幼,即便卵巢坏死,萎缩皮质仍可能具有内分泌功能,故予以保留,未切除右侧附件,行右侧腹股沟斜疝疝囊高位结扎术。
讨论
在胎儿生长发育的过程中,部分腹膜外翻形成鞘状突,出生后8月左右若鞘状突不闭合或闭合不完全,则易形成腹股沟疝,疝内容物通常是活动度大的脏器或组织,故以小肠等最为常见,疝内容物为附件者临床少见,亦见有内容物为子宫的临床报道。尤其需要注意的是,子宫及附件嵌顿后患儿常无肠管嵌顿后所致的呕吐、便秘、腹胀等梗阻症状,容易被忽略,易延误治疗,造成严重后果,如本组例2患儿发生卵巢坏死,高频超声能清晰显示疝内容物与腹腔器官的关系,从而明确疝内容物的成分协助临床治疗。超声医师应当提高对女性婴幼儿发生该病的认知度,密切结合临床表现,注意与腹股沟肿大淋巴结、脂肪瘤及其他肿瘤等进行鉴别,从而为临床制定治疗方案及时提供图像依据。
原始出处:
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#嵌顿疝#
29
#腹股沟附件#
30
#疝#
35
#超声诊断#
32
#超声诊断#
23