Oncologist:老年侵袭性非霍奇金淋巴瘤(NHL)的临床结局、治疗毒性和医疗保健利用
2021-08-13 yd2015 MedSci原创
尽管平衡治疗效果和并发症风险对于老年侵袭性非霍奇金淋巴瘤(NHL)患者至关重要,但很少有研究描述这些患者的临床结局、毒性率和医疗保健利用率。因此,来自美国的研究团队开展了回顾性研究,评估≥65岁
尽管平衡治疗效果和并发症风险对于老年侵袭性非霍奇金淋巴瘤(NHL)患者至关重要,但很少有研究描述这些患者的临床结局、毒性率和医疗保健利用率。因此,来自美国的研究团队开展了回顾性研究,评估≥65岁侵袭性非霍奇金淋巴瘤(NHL)患者治疗开始6个月的临床特征、预后、治疗毒性、非计划住院率和ICU住院率。相关结果发表在Oncologist杂志上。
研究纳入295例患者,中位年龄为73岁(范围65 - 100岁); 96/295或32.5%的患者年龄在65岁至69岁之间;77/295或26.1%的患者年龄在70 - 74岁;59/295人(20.0%)的患者年龄在75 - 79岁;63/295(21.4%)患者为80岁以上。大多数患者接受CHOP治疗(194/295,65.8%),其次是EPOCH(50/295, 17.0%)和mini-CHOP(27/295, 9.2%),均伴或不伴利妥昔单抗。大约五分之一(53/295,18.0%)的患者接受了中枢神经系统预防。大多数患者(201/295,68.1%)接受了6个周期的全身治疗,大约4.5个月的治疗。

治疗和预后
总人群的ORR为86.9%(253/291),完全缓解(CR)率为84.2%(245/291)。中位随访时间为5.9年(3.8-8.4年),5年OS率为74.2%(95%CI68.4 -79.1)。
治疗后3-5级非血液学毒性的发生率为42.4%(125/295),4-5级非血液学毒性的发生率为8.1%(24/295)。在3-5级非血液学毒性中,最常见的包括发热性中性粒细胞减少(40.0%)和感染(33.6%)。3.9%(10/295)的患者因治疗毒性死亡,最常见的死亡原因是感染。总体而言,41.0%(121/295)的患者在治疗开始后的前6个月内意外入院,6.1%(18/295)的患者在治疗开始后的前6个月内入住ICU。在可评估的首次非计划住院患者中(n = 121),最常见的住院原因是发热性中性粒细胞减少(41.3%),其次是感染(28.1%),其他非癌症用药情况(13.2%)和症状(9.1%)。在所有患者中,14.9%(44/295)有治疗剂量减少和/或延迟。
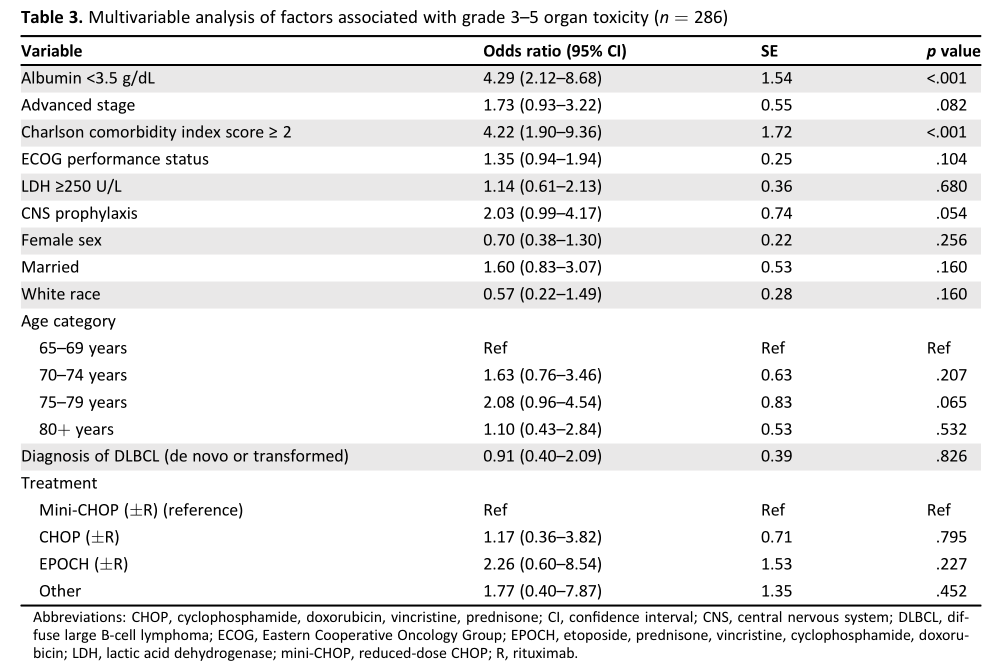
3-5级毒性相关因素
年龄在65-69岁、70-74岁、75-79岁和80岁以上的患者中,5年OS率分别为82.2% (95%CI, 72.4 -88.7)、72.0% (95%CI,59.7- 81.1)、73.6%(95%CI,59.2-83.6)和66.4%(95% CI, 52.5-77.0)。3-5级非血液学毒性分别为35.4%(34/96)、46.8%(36/77)、50.9%(30/59)和39.7%(25/63),4- 5级非血液学毒性分别为3.1%(3/96)、9.1%(7/77)、8.5%(5/59)和14.3%(9/63)。治疗开始后的前6个月内意外入院率分别为34.4%(33/96),45.5%(35/77),47.5%(28/59)和39.7%(25/63)。在治疗开始后的前6个月内入住ICU率分别为3.1%(3/96),5.2%(4/77),6.8%(4/59)和11.1% (7/63)。剂量减少率和/或剂量延迟率分别为12.5%(12/96)、16.9%(13/77)、13.6%(8/59)和17.5%(11/63)。
在多变量模型(n = 286)中,低白蛋白血症(OR, 4.29;95%CI, 2.12- 8.68;p<0.001)和高共病评分(OR, 4.22;95%CI, 1.90-9.36;p<0.001)都与更容易出现3-5级非血液学毒性。
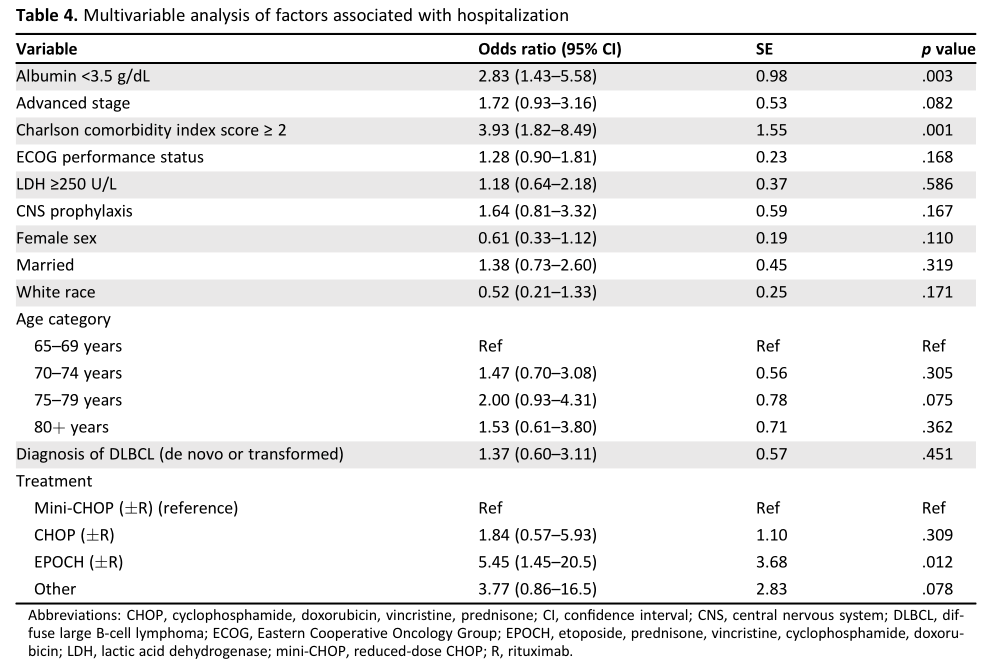
非计划住院的相关因素
在多变量模型(n = 286)中,低白蛋白血症(OR, 2.83;95%CI,1.43 -5.58;p = 0.003),高共病评分(OR, 3.93, 95% CI, 1.82-8.49;p = 0.001), EPOCH联合或不联合利妥昔单抗治疗方案(OR, 5.45;95%CI, 1.45-20.5;P =0.012)与高开始治疗后的前6个月计划外住院率相关。
综上,老年侵袭性非霍奇金淋巴瘤(NHL)治疗大部分存活超过5年,也有近一半患者经历毒性以及非计划住院。因此,对于这部分患者需要加强临床干预。
原始出处:
Johnson PC, Yi A, Horick N,et al. Clinical Outcomes, Treatment Toxicity, and Health Care Utilization in Older Adults with Aggressive Non-Hodgkin Lymphoma. Oncologist. 2021 Jul 29. doi: 10.1002/onco.13915. Epub ahead of print. PMID: 34327767.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#Oncol#
25
#临床结局#
44
#侵袭性#
42
#GIST#
37
#NHL#
52
#医疗保健#
42
谢谢梅斯分享这么多精彩信息
53