腹盆腔促纤维组织增生性小圆细胞肿瘤1例
2019-02-13 王汝佳 沈桂权 高波 医学影像学杂志
患者男性,18岁。主诉:发现腹部包块4个月。患者于4个月前因体检发现腹部包块,伴右上腹疼痛,间断性钝痛,有排便困难感,无腹痛、腹泻、血便、黑便等不适。
患者男性,18岁。主诉:发现腹部包块4个月。患者于4个月前因体检发现腹部包块,伴右上腹疼痛,间断性钝痛,有排便困难感,无腹痛、腹泻、血便、黑便等不适。
实验室检查:WBC:7.73×109,中性粒细胞百分比:68.10%,淋巴细胞百分比:20.60%,单核细胞百分比:7.50%,CA125:283.30U/ml,CA72-4:5.04U/ml。
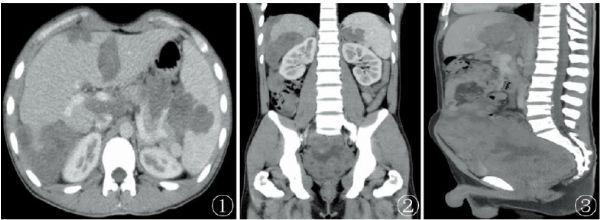
CT检查:患者腹盆CT增强表现如下(图1~3):腹膜、网膜、肠系膜、双侧膈肌、腹腔内、腹膜后、盆腔内、肝裂区、脾门见多发大小不等、结节样、团块样软组织密度影弥漫分布,边界不清,呈轻度不均匀强化,腹盆腔多发实质器官受侵,邻近肠道分界不清,病灶较大者位于盆腔膀胱-直肠间隙,最大截面约为106mm×134mm。
图1~3 CT增强(横断位+冠状位+矢状位)腹盆腔内多发不规则状软组织密度影,呈不均匀性强化,累及腹盆腔实质及空腔脏器
病理检查:患者行腹腔穿刺活检:考虑为促纤维组织增生性小圆细胞肿瘤,免疫组化为肿瘤细胞呈CK+,EMA+,Vimentin+,NSE局灶+,S-100局灶+,CD99+,Desmin+,WT-1+,CgA-,Syn-,LCA-,CD3-,CD20-,Myogenin-,MyoD1-,SMA间质+,Ki-67阳性率约30%(图4)。

图4 镜下见小圆形细胞,细胞核较小,核分裂像较多,细胞成巢状排列,周围被结缔组织所包饶(HE×400)
讨论:
促纤维组织增生性小圆细胞肿瘤(desmoplastic small round cell tumal,DSRCT)是一种罕见的可发生于腹盆腔内的具有高度恶性侵袭性的肿瘤,多见于青少年和年轻人。DRSCT于1989年被第一次报道。DSRCT没有确切的组织基因型和确切的生物学行为,遗传学和形态学特征迄今为止尚未被清楚地阐明。组织学上的特征是存在着被促纤维组织增生基质所包裹的未分化肿瘤细胞巢的出现。
CT是DSRCT最常用的检查方法,相对特异性的CT表现为:1)腹、盆腔内单发或者多发分叶状软组织肿块,边界清晰,但与肠系膜、网膜及腹膜分界不清;2)病灶与其周围脏器关系密切,但病灶主体部分常不位于任何实质或者空腔脏器内,因此难以判断其组织来源;3)部分患者肿块内可见多发斑点或小斑片状高密度钙化灶;4)一旦出现腹膜种植转移,腹膜则呈局限性或弥漫性增厚改变,可见团块状软组织肿物影附着于腹、盆壁;5)有些病灶可出现肝脏的多发转移,出现腹水的症状。
如果压迫输尿管,可引发肾盂积水的表现;压迫髂血管可导致下肢不适等一系列继发表现。目前DSRCT在影像学上报道的病例数目较少,造成影像诊断医师缺乏诊断经验,很难做出正确诊断。同时,也需要与其它肿瘤相鉴别,比如:横纹肌肉瘤、淋巴瘤、神经母细胞瘤、腹部原始神经外胚层肿瘤(PNET)、间皮瘤、腹膜平滑肌肉瘤、腹腔内纤维瘤病等。
原始出处:
王汝佳,沈桂权,高波,库媛.腹盆腔促纤维组织增生性小圆细胞肿瘤1例[J].医学影像学杂志,2018(01):5+15.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#腹盆腔#
85
#增生性#
58
想要积分
96