Pediatr Blood Cancer:放疗联合VPA和贝伐珠单抗治疗胶质瘤的耐受性良好
2021-12-16 MedSci原创 MedSci原创
高等级胶质瘤(HGG)和弥漫性固有树胶质瘤(DIPG)的预后仍然不乐观。理论上同时使用具有抗胶质瘤和放射增敏作用的药物应能改善HGG和DIPG的疗效。丙戊酸(VPA)是一种在儿童中使用了30多年的抗惊
高等级胶质瘤(HGG)和弥漫性固有树胶质瘤(DIPG)的预后仍然不乐观。理论上同时使用具有抗胶质瘤和放射增敏作用的药物应能改善HGG和DIPG的疗效。丙戊酸(VPA)是一种在儿童中使用了30多年的抗惊厥药,可以抑制组蛋白去乙酰化酶(HDAC),贝伐珠单抗是一种针对人血管内皮生长因子-A同种型的人源化单克隆IgG抗体,已被批准作为成人胶质母细胞瘤的治疗方法。新的一项2期临床试验中,研究人员评估了VPA和放疗,然后再用VPA和贝伐珠单抗治疗新诊断的DIPG或HGG患儿的疗效和耐受性,研究结果已发表于Pediatr Blood Cancer。
从2009年9月至2015年8月,研究纳入38名3~21岁的DIPG和HGG儿童患者(DIPG组20名,HGG组18名),接受放疗和VPA,剂量为15mg/kg/天,并调整剂量以维持在85~115μg/mL的谷值范围。放射后继续使用VPA,并在完成放疗后四周开始使用贝伐单抗,剂量为10 mg/kg,每两周静脉注射一次。
结果显示,在放疗和VPA期间,需要停止或修改VPA剂量的≥3级不良反应包括3级血小板减少(1)、3级体重增加(1)和3级胰腺炎(1)。在VPA和贝伐单抗期间,最常见的≥3级不良反应是3级中性粒细胞减少(3),3级血小板减少(3),3级疲劳(3)和3级高血压(4)。两名患者在疾病进展前停止了方案治疗(一名4级血栓形成,一名1级腔内出血)。
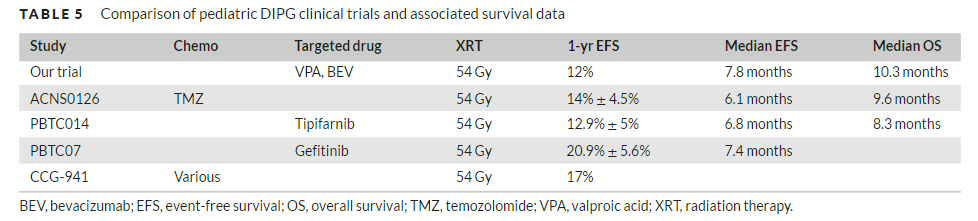
DIPG组中位无事件生存期(EFS)和总生存期(OS)分别为7.8(95% CI 5.6-8.2)和10.3(7.4-13.4)个月,估计一年EFS为12%(2%-31%)。HGG组中位EFS和OS分别为9.1(6.4-11)和12.1(10-22.1)个月,估计一年EFS为24%(7%-45%)。4例胶质母细胞瘤和错配修复缺陷综合征患者的EFS分别为28.5、16.7、10.4和9个月。
综上所述,该研究结果表明,放疗联合VPA和贝伐珠单抗的耐受性良好,但是似乎并不能改善DIPG或HGG儿童的EFS或OS。
原始出处:
Jack Meng-Fen Su, et al., A phase 2 study of valproic acid and radiation, followed by maintenance valproic acid and bevacizumab in children with newly diagnosed diffuse intrinsic pontine glioma or high-grade glioma. Pediatr Blood Cancer. 2020 Jun;67(6):e28283. doi: 10.1002/pbc.28283.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#DIA#
64
#PE#
63
#贝伐珠#
69
#耐受性#
100
#贝伐#
65