JACC:静脉注射药物相关心内膜炎的临床预后研究
2019-02-13 MedSci MedSci原创
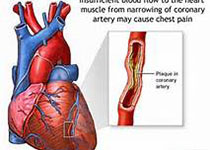
近年来由于静脉注射药物(IDU)使用的增多引起感染性心内膜炎(IE)住院率增高,本研究的目的旨在评估IDU-IE的趋势及临床预后。本研究纳入了2010-2015年NRD数据库中的IE患者,主要终点事件是30天再住院率和原因,次要终点事件包括死亡率、住院时间、费用和180天再住院率。最终,共纳入了96344名(77.8%)非IDU-IE患者和27432名(22.2%)IDU-IE患者,2010-20
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#静脉注射药物#
75
#内膜#
81
#JACC#
0
#静脉#
76
#ACC#
63
#心内膜炎#
65
#静脉注射#
0
#临床预后#
64