Radiology:DWI在幼年特发性关节炎中的应用
2021-05-08 shaosai MedSci原创
儿童幼年特发性关节炎(JIA)通常患有自身免疫介导的滑膜炎症。滑膜炎症可导致关节疼痛、僵硬、功能受损,最总导致生活质量下降。
儿童幼年特发性关节炎(JIA)通常患有自身免疫介导的滑膜炎症。滑膜炎症可导致关节疼痛、僵硬、功能受损,最总导致生活质量下降。即使由儿童风湿病专家进行检测,在临床检查中检测炎症(例如关节炎)的可靠性也十分有限。
尽管MRI尚未成为JIA疾病活动性预后指标的一部分,但有望成为评估小儿风湿病炎症活动性的重要工具。多项研究表明,增强MRI在滑膜炎症的显示及检测方面效果可靠。然而,增强MRI在JIA中的广泛应用受到以下几个因素的限制:较长的成像时间、较高的成本以及对比剂的使用导致的过敏反应、肾源性系统性纤维化以及钆在脑组织中的沉积。扩散加权成像(DWI)无需使用造影剂,且可根据水分子的不同扩散特征进行滑膜和关节积液的鉴别。然而据我们所知,尚未有研究关注DWI在检测关节炎和滑膜炎症中的诊断性能。
近日,发表在Radiology杂志的一项研究与临床参考标准相比,探讨了DWI对关节炎的诊断准确性,并比较了DWI与增强MRI对滑膜炎症的检测效能,为临床提供了一个扫描速度更快、更经济、无需造影剂的监测疾病活动性的MRI检查手段。
本项前瞻性研究纳入了45名患有幼年特发性关节炎(JIA)或疑似患有JIA的患儿(7名男孩,38名女孩;年龄中位数为14岁)。每位患者均接受了膝关节造影前和造影后的包括DWI序列的3.0T MRI检查。多学科小组根据临床、实验室和影像学表现(不包括DWI)确定是否存在关节炎,以作为临床参考标准。两组数据由两名对所有临床数据均不知情的放射科医生进行独立评分;数据集1包含强化前和强化后的MRI序列(增强MRI),数据集2包含强化前和DWI序列(DWI)。通过比较DWI数据集和临床参考标准的得分来确定诊断准确性。将DWI与增强MRI序列进行比较评估滑膜炎症的检测。
DWI检测关节炎的敏感性为93%(95%CI: 64%,100%),特异性为81%(95%CI:62%,92%)。45名参与者中有37人(82%)在DWI和增强MRI上对滑膜炎症的评分一致,结果敏感性为92%(13名参与者中有12人;95% CI: 62%,100%),特异性为78%(32名参与者中有25人;95% CI: 60%,90%)。

表 参与者的人口学和临床特征。
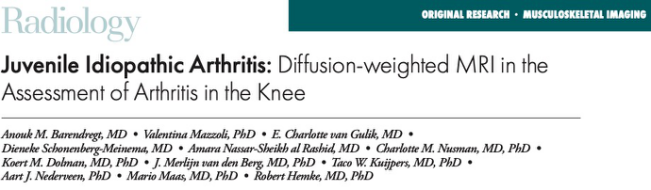
图1 (a) 14岁女孩,少关节扩展型幼年特发性关节炎(JIA)。在DWI数据集上,十字韧带周围可见滑膜炎症的表现。多学科小组(参考标准)决定该患者没有关节炎。箭头表示推测的滑膜炎症区域。(b) 10岁女孩,多关节类风湿性因子阴性JIA。在DWI数据集中,滑膜出现炎症。然而,多学科小组(参考标准)认定该患者没有关节炎。这一决定是基于(a)该患者早期MRI增强扫描显示交叉韧带周围有明显的滑膜炎症,而当前增强MRI扫描显示滑膜厚度明显变薄,以及(b)体格检查轻度异常。箭头表示推测的滑膜炎症区域。
综上所述,扩散加权成像(DWI)可以准确地检测患有幼年特发性关节炎(JIA)或疑似患有JIA的患儿,并与增强MRI性能相当。本研究结果表明,对于滑膜炎症的显示及检测方面,DWI可以作为增强MRI的代替成像手段,为临床提供一个无需造影剂的更便捷的影像学手段。
原文出处:
Anouk M Barendregt,Valentina Mazzoli,E Charlotte van Gulik,et al.Juvenile Idiopathic Arthritis: Diffusion-weighted MRI in the Assessment of Arthritis in the Knee.DOI:10.1148/radiol.2020191685
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#特发性#
47
学习学习
78
#关节炎#
56
#DWI#
53
学习学习
72