Cancer:精准医疗中,骨活组织检查在晚期前列腺癌中的分析
2017-12-26 AlexYang MedSci原创
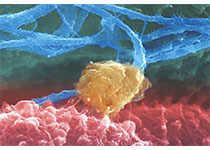
转移性活组织检查在患有晚期前列腺癌病人中越来越流行,主要目的是搜寻起作用的靶标和/或者鉴定出现的抗性机制。由于骨转移和它们硬化性质,获得足够的组织用来临床和基因组研究仍具有挑战。研究人员在2013年2月和2017年3月之间,募集了患有前列腺癌骨转移的病人,从而进行前瞻性的成像阴道的骨组织活检。研究人员搜集了新鲜的骨组织和血凝块。密质骨用添加了脱钙剂的福尔马林浸泡,进一步用于诊断。骨髓和血凝块在最优
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#期前列腺癌#
120
#活组织检查#
86
#精准#
92
#晚期前列腺癌#
82