JAMA Psychiatry:心血管疾病加重精神分裂症患者认知功能障碍
2021-03-18 MedSci原创 MedSci原创
合并代谢综合征、糖尿病和高血压等心血管疾病会加重精神分裂症患者的整体认知及个别认知领域障碍。
精神分裂症是一种脑部疾病,属于严重的精神障碍之一,每100人中便有一人患病。精分患者多于年轻时首次发病,但任何年龄段都有患病可能,男女比例无明显差异。很多人都误以为精分患者为多重性格或性格分裂,因此耽误了精分的治疗。
然而,即使是患者家属也有往往缺乏心理健康常识,对患者的表现表现的不知所措。实际上,患者仅有一种性格,但却会影响其精神和思想,从而导致行为表现异常。精分是可以医治的,但由于未及时就诊等原因,患者复发的机会较高。
此外,精神分裂症与认知功能障碍和心血管危险因素有关,包括代谢综合征(MetS)及其它代谢紊乱。认知功能障碍和心血管危险因素可使普通人群的认知恶化,并可能导致精神分裂症的认知障碍。
那么,精分患者的心血管疾病危险因素,如MetS及其构成障碍与精神分裂症的认知障碍之间是否有显著关联?为此,来自日本、美国、法国和新加坡等多个国家的精神卫生领域专家开展了相关研究,结果发表在最新的《美国医学会杂志》子刊JAMA Psychiatry上。
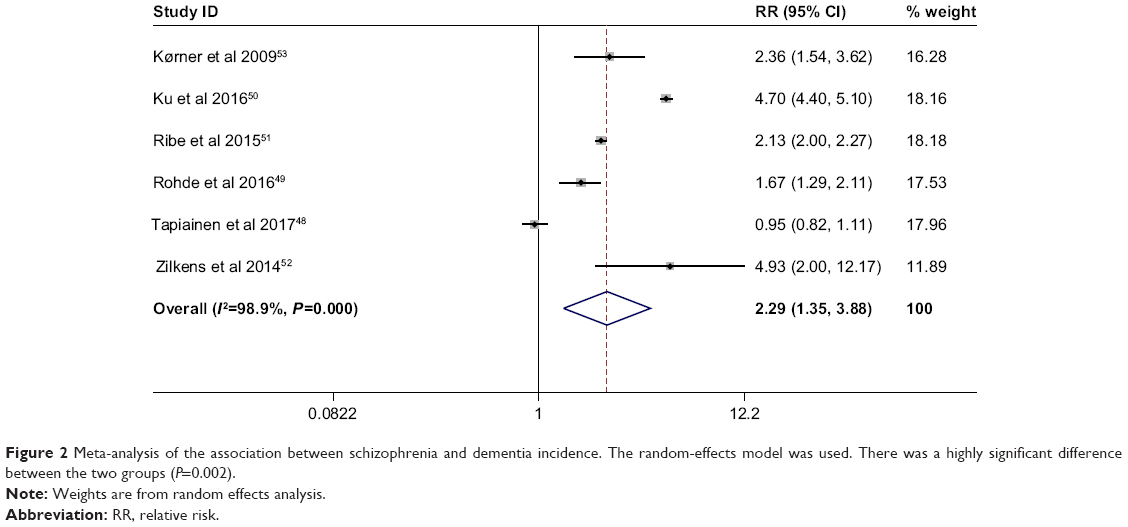
研究人员对Embase、Scopus、MEDLINE、PubMed和Cochrane数据库进行了搜索,纳入了以下研究:(1)检查精神分裂症或精神分裂症患者的认知功能;(2)调查心血管疾病危险因素,包括MetS、糖尿病、肥胖、超重、肥胖或超重、高血压、血脂异常和胰岛素抵抗与结果的关系;(3)比较有与无心血管疾病危险因素的精神分裂症/精神分裂症患者的认知功能。
共纳入了涉及10174名精神分裂症患者的27项研究。研究的主要结果是患者的整体认知情况,后者根据临床有效的整体认知功能测量的测试分数判断。
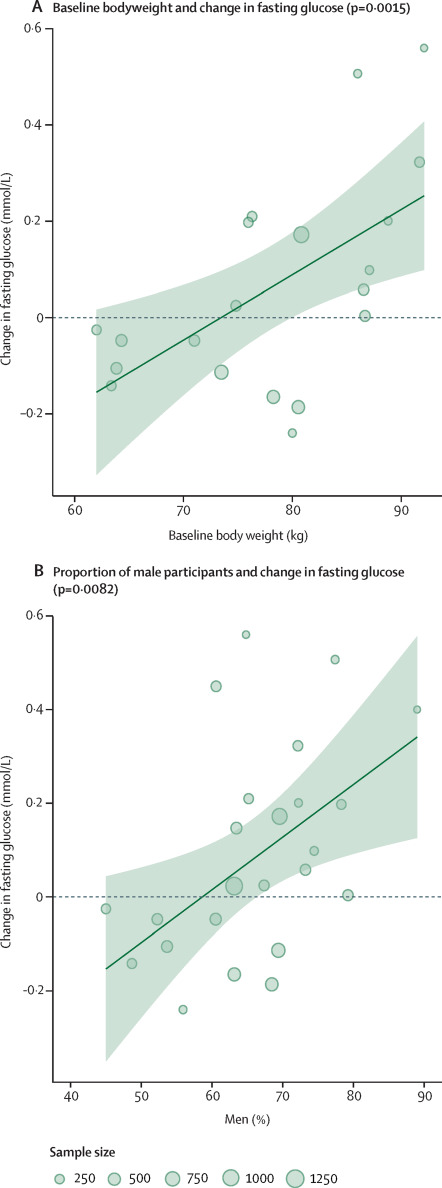
结果显示,患有MetS(13项研究;n = 2800)、糖尿病(8项研究;n = 2976),或高血压(5项研究;n = 1899)的精神分裂症患者认知功能整体较差;而肥胖(8项研究;n = 2779)、超重(8项研究;n = 2825)和胰岛素抵抗(1项研究;n = 193)的患者认知下降没有明显差异。
进一步分析显示,精神分裂症患者在特定认知领域的表现较差与认知功能障碍及心血管风险因素有关。其中合并糖尿病使得患者5个认知领域表现更差,而MetS和高血压则分别与4个认知领域表现更差有关。
综上,该研究表明,合并代谢综合征、糖尿病和高血压等心血管疾病会加重精神分裂症患者的整体认知及个别认知领域障碍。
参考文献:
Hagi K, et al. Association Between Cardiovascular Risk Factors and Cognitive Impairment in People With Schizophrenia: A Systematic Review and Meta-analysis. JAMA Psychiatry. Published online March 03, 2021. doi:10.1001/jamapsychiatry.2021.0015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Psychiatry#
36
#精神分裂#
39
#功能障碍#
28
#血管疾病#
33
科技进步,时**展。
69
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
39
学习了
62