JAHA:ACEi/ARB与COVID-19住院患者结局之间的关系
2022-05-23 MedSci原创 MedSci原创
在COVID-19住院的患者中,ACEi/ARB治疗与较低的炎症水平和较低的住院结局风险相关。需要进一步的临床试验来明确ACEI/ARB在COVID-19治疗中的作用。
到2021年6月,COVID-19全球大流行已导致全球超过1.7亿确诊感染病例和超过370万人死亡。血管紧张素转换酶抑制剂和血管紧张素受体阻滞剂(ACEi/ARB)的使用被认为通过调节血管紧张素转换酶2(SARS-CoV2的细胞进入受体)的水平来影响COVID-19的患病情况。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员试图评估因COVID-19住院患者的ACEI/ARB、炎症生物标志物和患者结局之间的关联。
研究人员利用国际COVID-19炎症研究(ISIC)确定了2020年2月1日至2021年6月1日期间因有症状的COVID-19入院患者,并评估了院内使用ACEI/ARB以及全因死亡、需要通气和需要透析之间的关联。研究人员使用连续测量的血压和血清肌酐值的边际结构模型估计了ACEi/ARB对复合结局的因果效应。
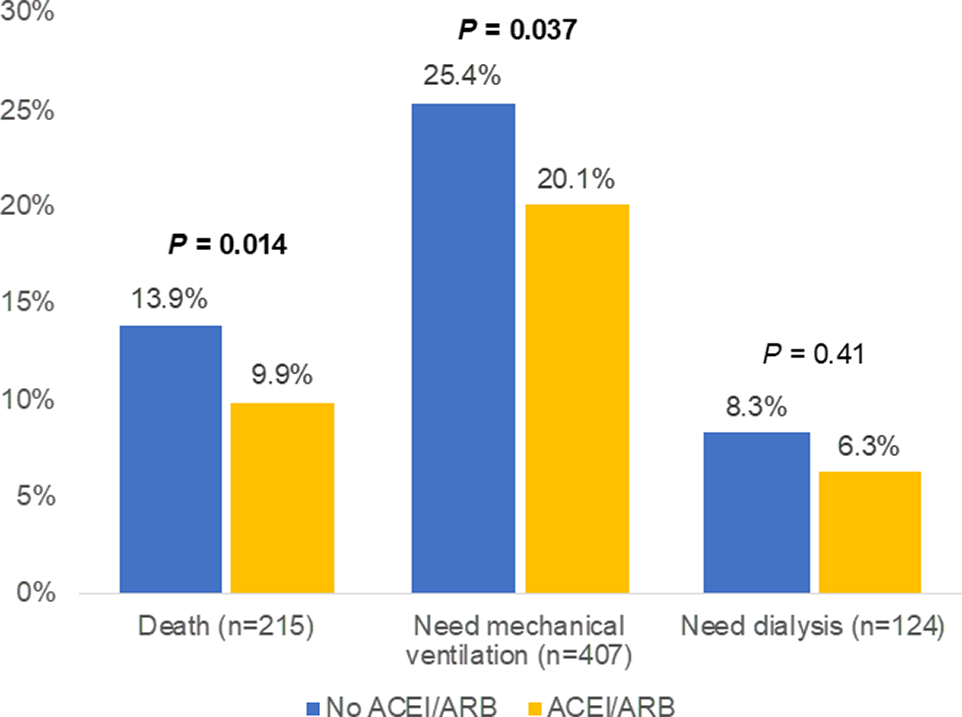
在ISIC研究的2044名患者中,1686名患者符合纳入标准,其中398名(23.6%)患者在COVID-19住院期间至少接受了1次ACEI/ARB治疗。该研究的参与者中有215人死亡,407人需要机械通气,124人在住院期间需要透析。既往使用ACEi/ARB治疗与较低水平的可溶性尿激酶纤溶酶原激活剂受体和C反应蛋白相关。在多变量分析中,院内使用ACEI/ARB治疗与较低的院内死亡、机械通气或透析复合结局风险相关(调整后的风险比为0.49,95%CI[0.36–0.65])。
由此可见,在COVID-19住院的患者中,ACEi/ARB治疗与较低的炎症水平和较低的住院结局风险相关。需要进一步的临床试验来明确ACEI/ARB在COVID-19治疗中的作用。
原始出处:
Michael Pan,et al.Angiotensin‐Converting Enzyme Inhibitors, Angiotensin II Receptor Blockers, and Outcomes in Patients Hospitalized for COVID‐19.JAHA.2021.https://www.ahajournals.org/doi/10.1161/JAHA.121.023535
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#ACE#
89
#AHA#
82
#患者结局#
61
赞赞赞😁
88
好难
88