NEJM:低-中SYNTAX评分的左主干病变患者接受PCI 的3年临床预后不劣于搭桥
2016-12-15 许菁 中国循环杂志
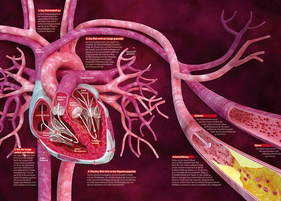
美国哥伦比亚大学 Gregg W. Stone等在新英格兰医学杂志发表研究显示,低-中SYNTAX评分的左主干病变患者接受PCI 的3年临床预后并不劣于搭桥。本组数据显示,PCI组的3年主要终点事件(全因死亡、脑卒中或心肌梗死)发生率为 15.4%,搭桥组为 14.7%,两组无差异。30 天内死亡、 脑卒中或心肌梗死的次要终点事件发生率在PCI组为 4.9%,显著低于搭桥组(7.9%)。3 年次要
美国哥伦比亚大学 Gregg W. Stone等在新英格兰医学杂志发表研究显示,低-中SYNTAX评分的左主干病变患者接受PCI 的3年临床预后并不劣于搭桥。
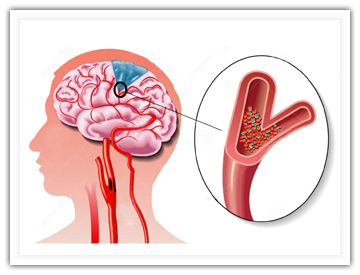
本组数据显示,PCI组的3年主要终点事件(全因死亡、脑卒中或心肌梗死)发生率为 15.4%,搭桥组为 14.7%,两组无差异。
30 天内死亡、 脑卒中或心肌梗死的次要终点事件发生率在PCI组为 4.9%,显著低于搭桥组(7.9%)。
3 年次要终点事件(死亡、 脑卒中、 心肌梗死或心肌缺血所致血运重建)发生率在 PCI组为 23.1%,搭桥组为19.1%,两组无差异。
研究纳入 1905例左主干病变患者,948 例患者接受PCI,957 例接受搭桥。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#搭桥#
62
#SYNTAX评分#
65
#左主干#
80
期待更长时间随访结果
100
#临床预后#
94