美新临床实验政策引担忧
2018-01-27 张章 科学网
近日,美国基本行为研究人员将迎来一项新政策。该政策为其联邦资助研究引入了若干新的规定,其中许多研究是美国国家卫生研究院(NIH)正在考虑的临床实验。许多研究人员认为这项政策毫无意义,而且会妨碍他们的工作。不过,NIH官员最近提出的修订版本减轻了人们的一些担忧。
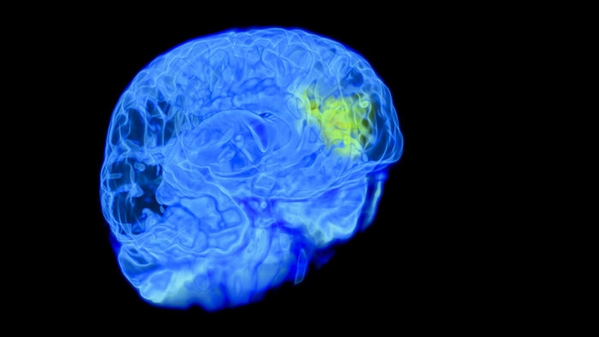 美国立卫生研究院或将脑部扫描研究定义为临床实验。图片来源:Thierry Berrod, Mona Lisa Production/Science Source
美国立卫生研究院或将脑部扫描研究定义为临床实验。图片来源:Thierry Berrod, Mona Lisa Production/Science Source本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#临床实验#
60
学习了.谢谢分享.
78
学习了.谢谢分享
88
#政策#
65
好好文章学习了
96