JCEM:靶向11- β羟化酶[131I]IMAZA -一种治疗晚期肾上腺皮质癌的新方法
2021-12-22 从医路漫漫 MedSci原创
肾上腺皮质癌(ACC)是一种预后不良的罕见恶性肿瘤。即使在完全切除后,仍有40-70%的患者出现疾病复发。到目前为止,药物治疗成功有限。目前治疗不可切除ACC的标准药物包括米托坦,它是唯一被批准的药物
肾上腺皮质癌(ACC)是一种预后不良的罕见恶性肿瘤。即使在完全切除后,仍有40-70%的患者出现疾病复发。到目前为止,药物治疗成功有限。目前治疗不可切除ACC的标准药物包括米托坦,它是唯一被批准的药物。基于大型三期试验的结果,米托坦经常结合依托泊苷、阿霉素、顺铂治疗。然而,这种联合治疗会导致23%的客观有效率,5.1个月的无进展生存期(PFS),并且与显著的毒性相关。因此,大多数患者需要二线和三线治疗方案。放射治疗在辅助治疗和姑息治疗两方面都有临床应用价值,表明ACC具有辐射敏感性。
目的:肾上腺皮质癌(ACC)是一种罕见的内分泌恶性肿瘤,治疗方法有限。肾上腺特异性放射示踪剂的治疗方法为改善诊断和治疗提供了希望。在此,我们报道了一种新的治疗急性ACC的方法,应用(R)-1-[1-(4[123I]碘苯基)乙基]- 1h -咪唑-5-羧酸氮杂基酰胺([123I]IMAZA)进行影像学诊断,应用[131I]IMAZA进行放射性核素治疗。放射性示踪剂[11C]美托咪酯和[123I]碘化咪酯([123I]IMTO)选择性结合肾上腺特异性酶11- β -羟化酶(CYP11B1)和醛固酮合酶(CYP11B2),并已被证明在肾上腺皮质癌组织中可以积累。利用这种高肾上腺皮质性,引入了一种治疗概念,使用[123I]IMTO进行分子成像,[131I]IMTO进行放射性核素治疗。
患者和治疗:在2014年12月至2019年6月期间,对69例不可切除的ACC和转移性疾病患者进行筛查,以确定[123I]IMAZA在已知肿瘤表现部位的特异性保留。在静脉注射约185 MBq [123I]IMAZA后,SPECT/CT观察到靶摄取。13例患者在所有ACC病变中表现出强烈的摄取,被一个跨学科肿瘤委员会认为适合使用[131I]IMAZA治疗。根据实体瘤疗效评价标准,所有患者均有可测量的目标病灶(RECIST版本1.1)。患者特征见表1。在前7种治疗的基础上,采用~ 75 MBq [131I]IMAZA剂量学来评估最大给药治疗活性。分别于注射后5 min、1、4、24、48、72-120 h采集全身平面图像。成像同时采集标准活动以进行质量控制。同时,采集血液样本以量化外周血中的活性浓度。推导了活性时间函数和停留时间,并确定了推荐的对血液的辐射吸收剂量。在非肾上腺皮质组织中没有[131I]IMAZA积累,血液被认为是实际危险的关键器官,即骨髓的替代。以2gy的骨髓剂量为目标,计算其最大耐受活性。对于之后的治疗,最大耐受活性是根据[123I]IMAZA测量的活性动力学来估计的。肿瘤疗效评价依据实体瘤疗效评价标准(RECIST版本1.1),不良反应评价依据常见毒性评价标准(版本5.0)。
结果:筛查后,13例患者接受[131I]IMAZA治疗,中位数为25.7 GBq(范围为18.1 - 30.7 GBq)。5人接受了第二疗程。最好的反应是两名患者的RECIST靶病灶减少了26%。5例病情稳定患者的中位生存期无进展,为14.3个月(范围8.3-21.9)。治疗后所有患者的中位总生存期为14.1个月(4.0-56.5)。治疗耐受性良好,即未观察到严重毒性反应(CTCAE分级≥3)。
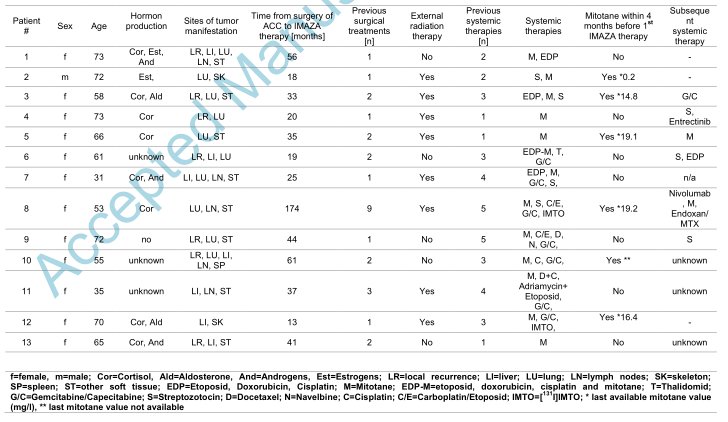
表1 13例晚期ACC患者特点分析
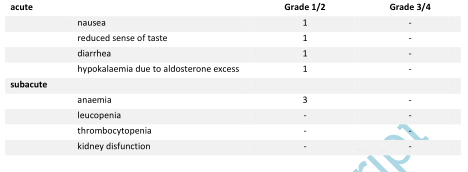
表2 根据CTCAE,[131I]IMAZA治疗后的急性和亚急性不良反应

表3 个体患者对[131I]IMAZA治疗的反应
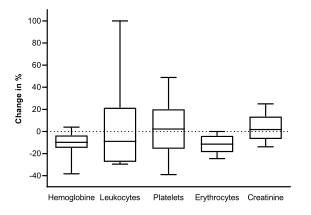
图1 [131I]IMAZA治疗后3个月血液参数的相对变化

图2 根据RECIST 1.1标准的靶区最佳反应:靶区最大直径(SOD)与基线之和的变化(以百分比表示)。绿色的患者表示病情稳定,而红色的患者表示疾病进展。患者13失去随访。仅因新病变而进展性疾病的患者标有*。
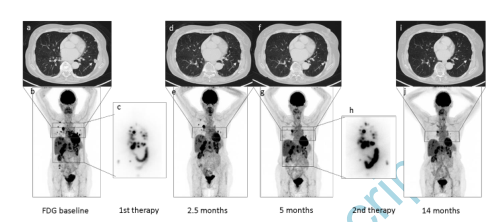
图3 1号患者在使用[131I]IMAZA两次治疗后的FDG-PET/CT扫描反应评估基线(a)、2.5个月、5个月和14个月(d, f, I,白色箭头)时肺转移的轴向ct切片。FDG-PET MIP在基线(b), 2.5个月,5个月和14个月后(e, g, j)。治疗后第1次治疗后4天(c)和第2次治疗后5天(h)的全身显像显示FDG-PET/CT示踪物聚集一致。
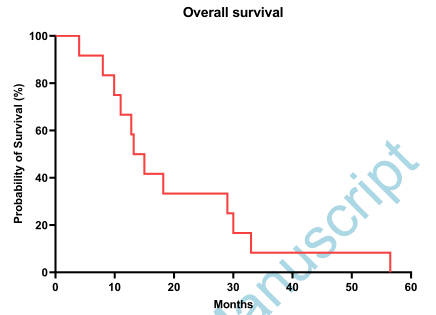
图4 总体生存率的Kaplan-Meier曲线。
结论:在标准治疗方案难以治疗的晚期ACC患者中,[131I]IMAZA治疗与疾病稳定、肿瘤大小在显著的患者比例中无显著减小以及治疗毒性相关。在38.5%的晚期ACC患者的肿瘤病灶中观察到较高的[131I]IMAZA摄取,这使得[131I]IMAZA在有限的、明确的患者中成为一种潜在的治疗选择。需要进一步的临床试验来评估这种新型治疗方法的全部潜力。
原文出处:
Hahner S, Hartrampf PE, Mihatsch PW,et al.Targeting 11-beta hydroxylase with [ 131I]IMAZA - a novel approach for the treatment of advanced adrenocortical carcinoma.J Clin Endocrinol Metab 2021 Dec 14
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#AZ#
133
#肾上腺皮质癌#
89
#JCEM#
88
#JCE#
82
#肾上腺#
97
#新方法#
86
点赞
78