专访|陆信武:颈动脉狭窄需防中风,微创新技术拆除主动脉瘤
2017-06-04 肖蓓 澎湃新闻
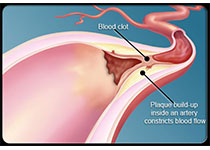
主动脉夹层、主动脉瘤,是致死率非常高的疾病,犹如一颗“不定时炸弹”,随时威胁患者生命。近三十年,随着血管外科的兴起,微创介入手术逐渐取代传统的开胸大手术,通过在血管内放置支架来拆除这个随时会破裂的“炸弹”。上海交大医学院附属第九人民医院血管外科主任陆信武教授,就是专注于此类疾病的“拆弹专家”。他带领九院血管外科,在累及弓上分支的主动脉腔内修复术中,创造 “激光原位开窗技术”,取得了初步成果。他
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






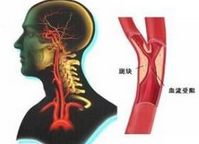






#颈动脉#
68
#新技术#
56
#专访#
53
#陆信武#
86
#创新#
54
#微创#
55
#主动脉#
60
#主动脉瘤#
46
#动脉狭窄#
63
非常好的文章,学习了,很受益
83