食管癌--X线钡餐-CT病例图片影像诊断分析
2022-09-06 华夏影像诊断中心 网络
食管癌是消化系统常见恶性肿瘤之一,好发于40岁以上,男性多见。临床上主要表现为进行性吞咽困难。病变部位:中段>下段>上段。病理上以鳞癌为多。食管癌可分为早期食管癌和中晚期食管癌。
【病史临床】男,63岁,胸痛,进行性吞咽困难伴消瘦20天。
【影像图片】
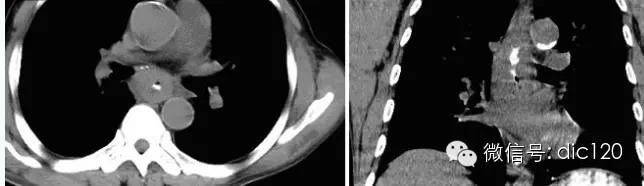

【影像表现】 CT:表现现为食管壁明显增厚,管腔狭窄;食管与周围结构分界不清食管吞钡:食管中段充盈缺损,管腔不规则狭窄,管壁僵硬,粘膜纠集破坏,与正常食管壁分界清晰。
【诊断】 病理诊断:食管(中下段)高-中分化鳞状细胞癌,侵及食管壁全层。(图1.2)
【鉴别诊断】
1.食管良性肿瘤(平滑肌瘤)
2.食管贲门失迟缓症
3.胃食管反流病
4.食管静脉曲张
【讨论】 食管癌是消化系统常见恶性肿瘤之一,好发于40岁以上,男性多见。临床上主要表现为进行性吞咽困难。病变部位:中段>下段>上段。病理上以鳞癌为多。食管癌可分为早期食管癌和中晚期食管癌,早期食管癌可分为隐匿型、糜烂型、斑块型和乳头状型。中晚期癌可分为5型,髓质型:呈坡状隆起,侵及食管壁各层及周围组织,本型多见,恶性程度较高。蕈伞型:多呈圆形或卵圆形,向食管腔内突起,边缘外翻如蕈伞状,表面常有溃疡,属高分化癌,预后较好。溃疡型:表面常有较深的溃疡,边缘稍隆起,出血和转移较早,梗阻发生较晚。缩窄型:环形生长,质硬,侵入食管全周,食管粘膜呈向心性收缩,梗阻发生较早,转移发生较晚,本型少见。其他类型:不能归入上述各型的。
影像学诊断要点:内镜检查并活检是诊断食管癌首选的方法。内镜下食管粘膜染色有助于提高早期食管癌的检出率。X线检查:早期食管癌:病变区黏膜皱襞增粗紊乱,中断及扭曲;小凹陷或隆起性病变,直径约<5mm,管壁轻度僵硬,扩张伸展稍受限。可形成溃疡,呈地图状。病变常累及周径于局部,与正常管径分界截然。进展期:蕈伞型:管腔内菜花样或蕈伞样充盈缺损,偏于食管一侧,范围较大,可见不同程度梗阻。溃疡型:纵形腔外龛影,龛影可见尖角征,周边可见环堤(周围肿瘤组织呈带状密度减低区)。浸润型:局限性环形狭窄,轮廓毛糙,与正常食管分界清楚,钡剂通过缓慢,近端不同程度扩张。髓质型:广泛侵犯食管全层,形成腔外肿物,管腔狭窄,表面可见溃疡。混合型:以上多种表现均可存在。CT:食管壁环形或不规则增厚,厚度>5mm应视为异常;或形成腔内肿块,多为广基底,表面有时可见龛影;食管周围脂肪层模糊、消失;周围器官受累或(和)淋巴结转移;增强扫描可见肿块轻度强化,较大瘤体强化不均匀,可合并低密度坏死灶。MRI:扫描前需嘱咐病人吞服适量液体。中晚期食管癌表现为信号异常,T1WI与肌肉信号近似,T2WI较肌肉信号高,增强扫描病灶明显强化。
与食管贲门失弛缓症相鉴别:后者多见于20~40岁女性,临床上表现为间歇性吞咽困难,病程较长,典型X线钡餐表现为漏斗状或鸟嘴样梗阻,管壁柔软,边缘光滑,粘膜正常,食管上段明显扩张。服用硝酸甘油类药物可缓解症状。
与胃食管反流病相鉴别:后者影像学无新生物,仅表现为粘膜炎症、溃疡或糜烂。
与食管静脉曲张相鉴别:后者常有肝硬化、门脉高压病史,食管壁柔软,粘膜正常,CT增强扫描可见明显强化的迂曲血管团,呈持续、延迟性强化。MRI:由于流空效应,曲张的血管在T1WI及T2WI上均呈低信号,增强扫描静脉期病灶明显强化。CT三维重建及MRI血管重建可以清晰显示曲张血管的全貌。
与食管平滑肌瘤相鉴别:后者表现为腔内光滑圆形充盈缺损,无管壁僵硬、黏膜皱襞破坏、周围组织侵犯及转移等恶性肿瘤征象。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CT病例#
126
#X线#
82
#食管#
120
#影像诊断#
66