JACC:低密度脂蛋白胆固醇处于正常水平就安全了?
2017-12-13 MedSci MedSci原创
传统上认为,缺乏心血管危险因素(CVRFs)患动脉粥样硬化的风险低,然而,没有CVRFs的个体仍报道有不良心血管事件的发生。本研究的目的旨在评估分析没有CVRF的个体患亚临床动脉粥样硬化的危险预测因素。本研究纳入了PESA临床试验中无传统心血管危险因素的个体(n = 1,779; 平均年龄为45.0 ± 4.1 岁,女性占 50.3%)。无传统心血管危险因素包括一下几点:不吸烟,血压<140/90
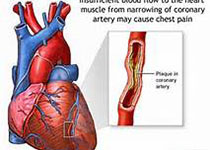
传统上认为,缺乏心血管危险因素(CVRFs)患动脉粥样硬化的风险低,然而,没有CVRFs的个体仍报道有不良心血管事件的发生。本研究的目的旨在评估分析没有CVRF的个体患亚临床动脉粥样硬化的危险预测因素。本研究纳入了PESA临床试验中无传统心血管危险因素的个体(n = 1,779; 平均年龄为45.0 ± 4.1 岁,女性占 50.3%)。无传统心血管危险因素包括一下几点:不吸烟,血压<140/90mm Hg,空腹血糖低于126毫克/分升,总胆固醇<240毫克/分升,低密度脂蛋白胆固醇(LDL-C)<160毫克/分升和高密度脂蛋白胆固醇≥40毫克/分升。其中,血压<120/80 mm Hg,空腹血糖<100毫克/分升,糖化血红蛋白<5.7%,总胆固醇<200毫克/分升的个体定义为最佳亚组(n=740)。评估分析的临床指标包括:超声检测颈动脉、髂股、腹主动脉斑块;冠状动脉钙化;血清标志物;生活方式。最终,发现有49.7%的无传统心血管危险因素的个体患有亚临床动脉粥样硬化(动脉斑块或冠脉钙化)。评估分析结果显示,男性、年龄和LDL-C与动脉粥样硬化呈独立相关性。此外,动脉粥样硬化同样与参与者
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#JACC#
45
谢谢分享学习了
85
#ACC#
36
#脂蛋白#
33
学习了很多先进的医疗技术
80
学习了.谢谢分享
67
谢谢分享学习了
78