Cell Research:小分子“魔法药水”体外实现人类原代肝细胞可逆转化和扩增
2018-10-29 上海交通大学 细胞
上海交通大学医学院附属仁济医院鄢和新教授和第二军医大学东方肝脏外科医院王红阳院士研究团队发表了最新原创性成果“Expansion and differentiation of human hepatocyte-derived liver progenitor-like cells and their use for the study of hepatotropic pathogens”, 这一研
肝细胞在体内具有强大的再生潜能,但多种致病因素导致肝脏细胞整体损伤和自我更新能力受损,若不加干预将逐渐演变急慢性肝衰竭。目前肝衰竭治疗仍以肝移植作为首选治疗手段,却因供体不足无法满足国内众多肝病患者的需求。近年基础与临床研究表明,肝细胞移植是治疗急慢性肝衰竭的有效方法,然而人类肝细胞无法在体外培养和扩增这一难题仍未解决,因此如何快速获得大量具有功能的肝细胞成为可供临床应用的关键。
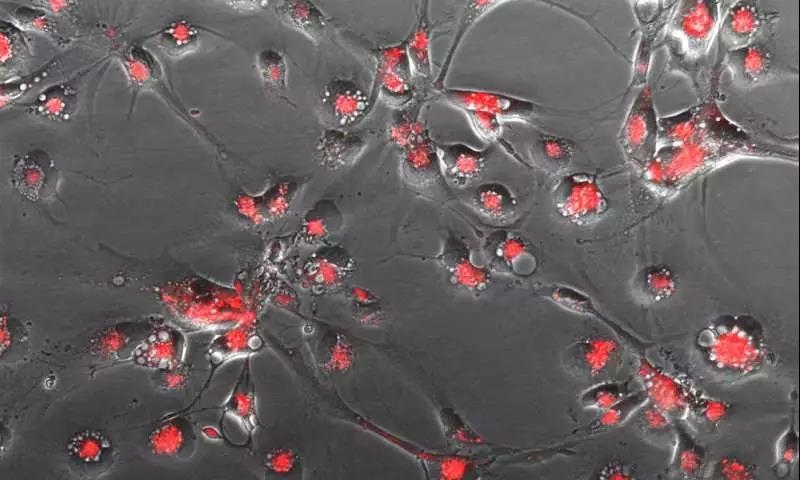
鄢和新教授/王红阳院士团队报道了其最新的研究成果:在改良的小分子重编程培养体系中,可在无任何外源基因导入的条件下,实现人类原代肝细胞向肝前体样细胞(Hepatocyte-derived liver progenitor-like cells,HepLPCs)的转化和快速扩增,并能重新分化为具有功能的肝细胞,实现人成熟肝细胞和肝前体样细胞之间的可逆转化。且在进一步研究中发现SIRT1介导的表观调控在肝细胞向肝前体样细胞的可逆转化和扩增中发挥重要作用。
肝前体样细胞HepLPCs在基础研究及临床应用方面展现了广阔前景。移植诱导分化的HepLPCs-Hep进入FAH基因缺陷联合免疫缺陷小鼠体内,并在小鼠血液中可检测到人特异性ALB和AAT分泌,实现有效地定植并重建受损肝脏,为首次通过移植体外扩增人肝细胞治疗代谢性肝病,这也提示我们通过自体或异体肝细胞移植替代原位肝移植,治疗急慢性肝损伤疾病可能。
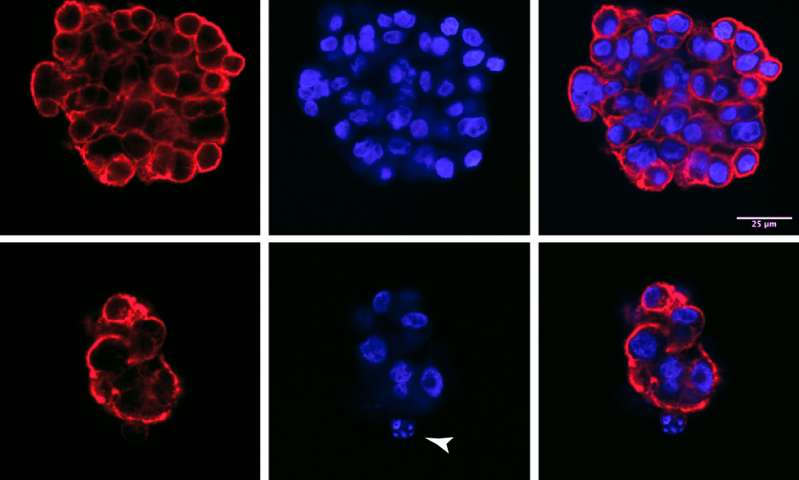
此外,HepLPCs在体外三维培养形成的类器官样组织球还可用于HBV感染与药筛研究,除验证了CRISPR/Cas9技术在HBV感染治疗中的潜在价值外,其对HBV稳定而长期的感染也有利于对HBV病毒更深入地观察和研究。
原始出处:
Fu GB1, Huang WJ1, Zeng M1, et al.Expansion and differentiation of human hepatocyte-derived liver progenitor-like cells and their use for the study of hepatotropic pathogens.Cell Res. 2018 Oct 25. doi: 10.1038/s41422-018-0103-x. [Epub ahead of print]
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#CEL#
55
#Cell#
59
#小分子#
64
#肝细胞#
61
学习了谢谢
69
#Research#
56