Neurology : Neurofascin-155免疫球蛋白亚型,临床病理关联和神经结局
2021-10-16 Freeman MedSci原创
NF155-IgG4(而不是IgM或IgG)患者具有独特的临床-电诊断特征
Neurofascin-155(NF155)自身抗体是最常见的结节和副结节抗体之一,占所有慢性脱髓鞘多发性神经病(CIDP)病例的4%至18%。尽管这些抗体在临床实践中的应用越来越多,但评估长期结果和组织病理学特征的研究是有限的。
藉此,梅奥诊所的Shahar Shelly等人, 探究了一个大型脱髓鞘神经病队列中NF155自身抗体的频率。并评估表型和组织病理学特异性,以及NF155-IgG4血清阳性、NF155泛IgG和NF155-IgM血清阳性病例之间的结果差异。最后,还比较了NF155-IgG4阳性病例与髓鞘相关糖蛋白(MAG)-IgM和Contactin-1 IgG相关脱髓鞘神经病的表型差异和结果。
方法。在这项研究中,对在梅奥诊所就诊的神经病患者血清进行了NF155-IgG4、NF155-IgG和NF155-IgM自身抗体的检测。对所有血清阳性病例的人口学和临床数据进行了回顾。
他们发现了32名NF155患者(25名NF155-IgG阳性[20名NF155-IgG4阳性],7名NF155-IgM血清阳性)。NF155-IgG4血清阳性患者临床上表现为远端肌无力多于近端肌无力,感觉症状阳性(刺痛、不对称性麻痹、神经性疼痛)和步态共济失调。许多人出现颅神经受累(11/20,55%)和乳头水肿(4/12,33%)。
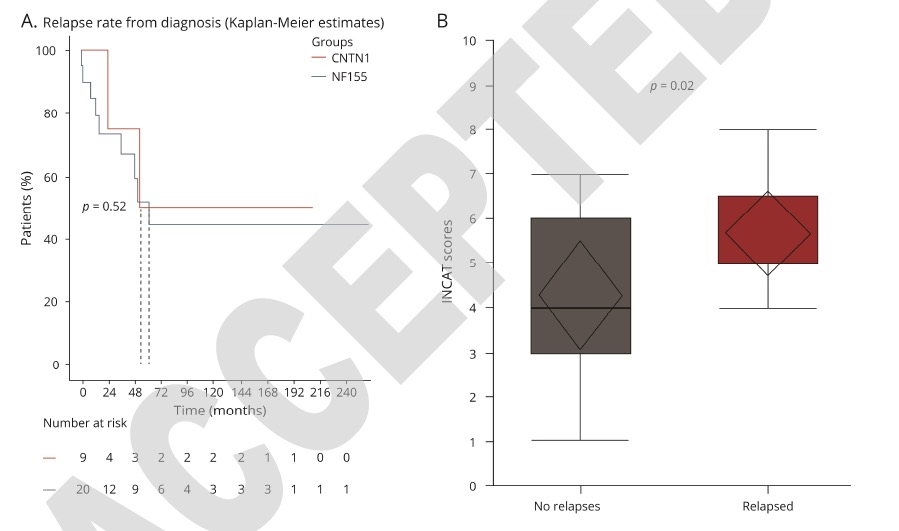
电诊断测试(EDX)显示脱髓鞘多发性神经病(19/20,95%)。45%的患者出现自主神经受累(9人,中位CASS评分3.5,范围1-7)。NF155-IgG4患者(n=11)的神经活检显示有分组的节段性脱髓鞘(50%),髓鞘重排(45%)和副节肿胀(50%)。大多数患者需要二线和三线的免疫抑制,但有良好的长期疗效(n=18)。在14名有2年以上连续EDX的患者中,除一人外,所有患者在治疗后都有改善。
NF155-IgG阳性的NF155-IgG4阴性(NF155-IgG阳性)和NF155-IgM阳性患者在表型上与NF155-IgG4血清阳性患者不同。
与MAG-IgM神经病相比,NF155-IgG4阳性患者的感觉共济失调、神经性疼痛、小脑功能障碍和根/神经丛MRI异常明显更常见。
与NF155-IgG4阳性病例相比,慢性免疫感觉多发性神经病(CISP)/CISP-plus表型在Contactin-1神经病中更常见。
与MAG-IgM血清阳性病例相比,NF155-IgG4阳性病例对免疫治疗反应良好,与接触素-1 IgG相比,远端获得性脱髓鞘对称性神经病(P<0.001),长期临床疗效更好(P=0.04)。
这个研究的重要意义在于发现了NF155-IgG4患者的长期随访和临床结果。NF155-IgG4(而不是IgM或IgG)患者具有独特的临床-电诊断特征。并证明NF155-IgG4阳性患者,与经典的CIDP不同,在发病时常见神经性疼痛和自律性失调。长期的结果是有利的。
原文出处:
Shelly S, Klein C, Dyck PJB, et al. Neurofascin-155 Immunoglobulin Subtypes: Clinicopathologic Associations and Neurologic Outcomes. Neurology. Published online October 11, 2021:10.1212/WNL.0000000000012932. doi:10.1212/WNL.0000000000012932
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#球蛋白#
61
#FAS#
69
#ASC#
67
#CIN#
63
#临床病理#
85
#Neurol#
0
#免疫球蛋白#
64