Cell Death Differ:IL-24缺失抑制IL-4诱导的巨噬细胞M2型转化以预防肺纤维化作用
2020-11-14 xiaozeng MedSci原创
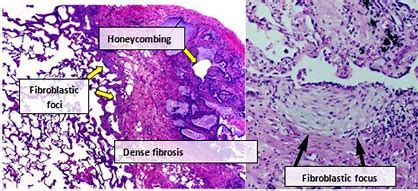
特发性肺纤维化(IPF)作为全球范围内的一种严重的健康问题,特发性间质性肺炎的最常见类型,预后较差。尽管IPF的发病率仅为每年2.8–18例/10万,但确诊后患者的平均生存期仅为2-4年。
特发性肺纤维化(IPF)作为全球范围内的一种严重的健康问题,特发性间质性肺炎的最常见类型,预后较差。尽管IPF的发病率仅为每年2.8–18例/10万,但确诊后患者的平均生存期仅为2-4年。然而IPF发生发展的分子机制仍是未知之数。
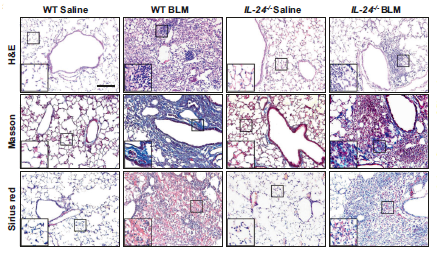
在该研究中,研究人员发现,在IPF患者的血清和博莱霉素(bleomycin,BLM)诱导的肺纤维化小鼠模型的支气管肺泡灌洗液(BALF)中均检测到IL-24(IL-20亚家族细胞因子成员)表达水平的升高。而缺失IL-24可以保护小鼠免受BLM诱导的肺损伤和纤维化作用。
IPF患者及BLM诱导小鼠模型中IL-24的表达分析
进一步的研究显示,IL-24缺失能够显著减少BLM诱导的小鼠肺中TGF-β1的产生,并减少M2型巨噬细胞的浸润。机制研究显示,单独的IL-24并不会对巨噬细胞向M2型转化产生明显的影响,而其与IL-4的协同作用则能够促进巨噬细胞的M2型转化作用。
IL-24缺失可减轻肺损伤和肺纤维化
研究人员发现,IL-24能够抑制IL-4诱导的细胞因子信号抑制因子SOCS1和SOCS3的表达水平,并增强了STAT6/PPARγ信号转导通路,最终促进IL-4诱导的M2型巨噬细胞的产生。
总而言之,该研究结果揭示了IL-24与IL-4的协同作用能够促进巨噬细胞向M2型转化,最终促进肺纤维化的发生发展。
原始出处:
Rao, L., Wang, Y., Zhang, L. et al. IL-24 deficiency protects mice against bleomycin-induced pulmonary fibrosis by repressing IL-4-induced M2 program in macrophages. Cell Death Differ (03 November 2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Differ#
109
#Cell#
73
#CEL#
74
IL-24与IL-4的协同作用能够促进巨噬细胞向M2型转化,最终促进肺纤维化的发生发展
138
#Death#
0
#IL-2#
84
已读
133
学习了
131
学习学习
133