Int Arch Allergy Immunol:皮下过敏原特异性免疫治疗对小儿过敏性鼻炎患者是安全的
2021-03-29 AlexYang MedSci原创
皮下过敏原特异性免疫治疗(SCIT)是治疗儿童过敏性鼻炎的主要疗法之一,其能够改善症状和生活质量,但也不能排除不良反应(ADVrs)。尽管如此,也有一些报告对其安全性进行了评价。
皮下过敏原特异性免疫治疗(SCIT)是治疗儿童过敏性鼻炎的主要疗法之一,其能够改善症状和生活质量,但也不能排除不良反应(ADVrs)。尽管如此,也有一些报告对其安全性进行了评价。

最近,有研究人员评估了儿童患者对SCIT的ADVr。

研究人员回顾了2005年至2018年的786份SCIT临床记录。研究发现,在786名患者中,有106名(13.4%)发生ADVrs。具有ADVr的患者至少有2种过敏原的敏感性和免疫治疗,与对照组(CG)相比具有显著差异(p<0.001),其中包含了标准化和非标准化过敏原的组合(p=0.003)。ADVrs处于蓄积期(p<0.001)。生存曲线显示,50%的人在SCIT治疗12周时有一些反应。最常见的ADVr为1级73/106(68.8%),33/106名患者为2级(31.1%)。WAO分级系统各等级之间的对数秩分析显示存在显著差异(P=0.02)。
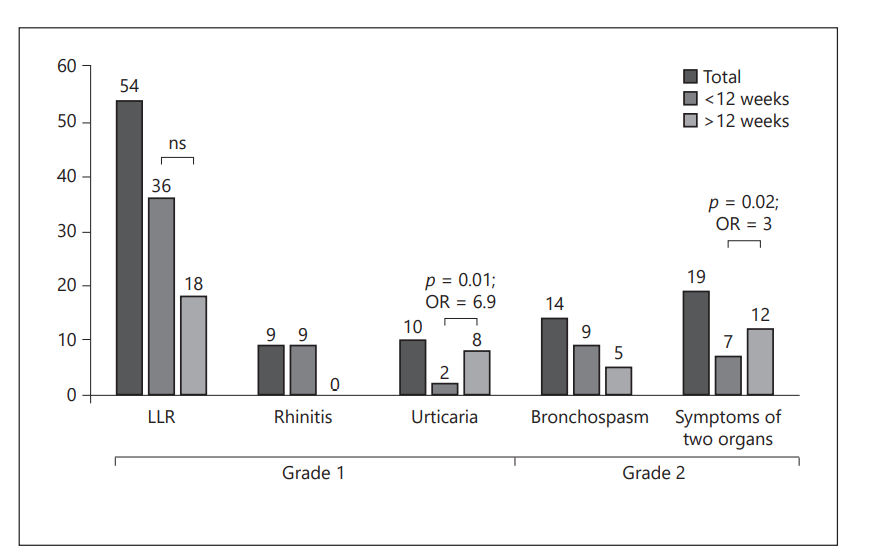
SCIT的ADVrs频率分析
最后,研究人员指出,SCIT在儿童患者中是安全的。ADVrs并不常见,报道最多的是1级;但在>12周时,涉及2个器官系统的ADVrs风险增加。
原始出处:
Gandhi F Pavon-Romero , Désirée E Larenas-Linnemann , Karen Eloisa Xochipa Ruiz et al. Subcutaneous Allergen-Specific Immunotherapy Is Safe in Pediatric Patients with Allergic Rhinitis. Int Arch Allergy Immunol. Feb 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#过敏性#
50
#特异性#
80
学到了
71
#ALL#
62
#过敏原#
67