Cell Metab:你知道吗?肥胖竟有多种类型,到底哪一种关乎你的健康呢?
2018-11-01 佚名 细胞
如今我们的社会似乎已经接受了这样一种观点,即体重增加是在一个容易摄入卡路里的环境中长大所产生的必然结果,然而在我们的职业和私人生活中,体育锻炼所起到的作用越来越小,而且衰老只会让减肥变得更加困难。
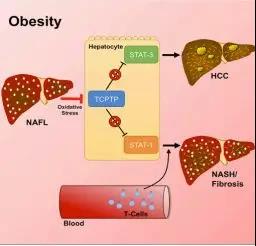
从短期来看,超重的后果似乎很遥远或者说并不重要,但其最终却会导致更高的糖尿病和心脏病发病率,而且还会对人类积极的生活方式提出重大挑战;笔者(斯克利普斯研究所的研究者Amalio Telenti)研究发现,肥胖或许并不仅仅是皮肤下的一些脂肪,其是机体新陈代谢的一种真正的改变;肥胖会改变机体处理营养物质的方式,也会改变维持机体生存的化学反应。
最近,一项刊登在国际杂志Cell Metabolism上的研究报告中,研究人员就通过研究分析了肥胖对机体代谢所产生的影响,他们认为,肥胖有多种类型,每一种对一个人的健康都会产生不同后果,这就是所谓的疾病异质性,如果我们能够深入理解这种异质性,或许就能开发出个性化的肥胖疗法,从而更加成功地对肥胖患者进行治疗。
肥胖,代谢组
笔者所带领的研究团队有着不同的学科背景,包括医学、技术以及复杂数据的分析等,研究人员利用两种强大的新型技术对近乎2500名肥胖个体进行了研究,对每一名参与者机体的基因组进行了测序,随后对1000多份血液样本中的化合物或代谢产物进行了分析。这种代谢产物的集合就是如今我们所说的“代谢组”,其包括众所周知的化合物,比如葡萄糖和尿酸以及诸如1-硬脂酰2-二同-亚连酰-GPC(1-stearoyl-2-dihomo-linolenoyl-GPC)等化合物。
研究人员对参与者机体的基因组进行分析,旨在理解每个人机体的基因是如何驱动其肥胖的分子机制,研究者选择代谢组来实时捕获超重对机体健康的影响,很多参与者都被追踪调查了10年以上,这就能够帮助研究人员能够评估参与者长期的健康后果。研究者发现,参与者机体中数百种特殊代谢产物的水平会受到体重改变的影响;其中一些变化是意料之中的,脂质(胆固醇)会随着体重增加而快速增加,然而研究者还观察到了机体中其它类型代谢产物及及生理性过程的变化,比如蛋白质和碳水化合物的代谢、能量产生及激素浓度的改变等。
总的来说,体重会极大地干扰机体的新陈代谢,但好消息是,这种变化是可以随着体重减轻而发生逆转的。
健康的肥胖者和不健康的瘦人
另一项基本的观察结果是,新陈代谢改变所带来的健康影响比单纯的身体方面或许影响更大,一些参与者的体重正常,但其机体中却携带有特殊的肥胖代谢产物,而一些肥胖个体的代谢组非常正常,其与那些拥有健康体重指数的个体非常相似。研究人员并不清楚为何肥胖个体会拥有正常的机体代谢组,他们也并不知道到底是基因还是环境会让这群人变得更加健康,当然这还需要后期更多的研究来阐明。
由于在进行代谢分析时研究者拥有相关的医学信息,而且还有长期的跟踪数据,因此研究者能够轻松看到参与者机体异常代谢所带来的结果。研究者表示,那些遭受最严重代谢异常的肥胖个体常常会患上糖尿病、心脏病和高血压等,这些参与者的腹部和肝脏中也会积累脂肪组织,而并不仅仅是腰部和臀部的皮下会积累脂肪组织;因此身体的肥胖很重要,但超重如何唯一地影响到每个人的机体活动或许是更准确衡量个体整体健康的一个标准。
代谢组报告或许比机体的BMI更加重要
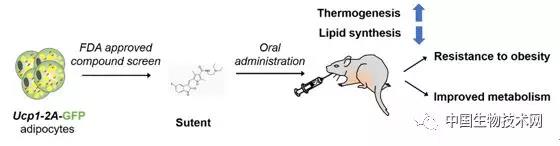
人们可能会很容易地认为肥胖是遗传了父母亲基因的结果,的确如此,但与高热量摄入及久坐不动的生活方式所带来的巨大影响相比,机体基因锁带来的影响就相形见绌了。有一个例外,研究人员发现,一些非常肥胖的个体机体中控制食欲的基因发生了改变,这种基因就是所谓的黑皮质素-4受体(MC4R),这些患者拥有的遗传突变会让其永远处于饥饿状态,并且会让其吃的比实际上需要的更多,研究人员希望能利用特殊的药物来治疗这类特殊的肥胖,正如所料,这种形式的肥胖也会严重干扰患者机体的新陈代谢。
研究者一直认为,科学会为重要的健康问题提供新的见解,具体到肥胖症的研究,研究者认为,关注机体新陈代谢的变化或许是未来的一个研究热点,这项工作能为研究人员提供方法来测定机体肥胖所带来的有害影响,并且对人群进行筛查找出哪些个体能因特殊的新药而获益,这其中就包括那些骨瘦如柴、机体代谢组不健康,但并不知道自身状况的人,这些个体或许能从早期的干预中获益。
原始出处:
Elizabeth T. Cirulli,Lining Guo,Christine Leon Swisher, et al. Profound Perturbation of the Metabolome in Obesity Is Associated with Health Risk. Cell Metabolism October 11, 2018. doi:10.1016/j.cmet.2018.09.022
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Cell#
55
#CEL#
56
#Meta#
59
#MET#
51
学习了谢谢了
87
有意思
93