JAHA:冷冻球囊消融对肺血管急性血流动力学和组织的影响!
2017-06-26 xing.T MedSci原创
由此可见,CB-PVI操作导致肺动脉和右心房压力显著上升,以及导致肺静脉壁损伤。这些研究结果的临床意义值得进一步研究。
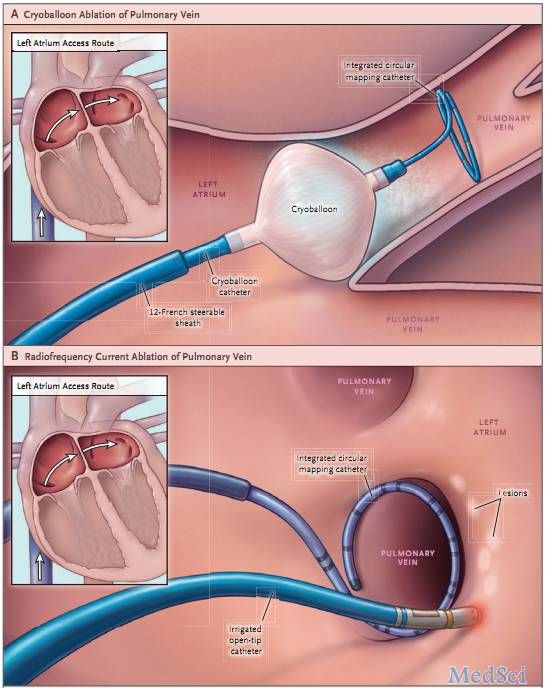
基于冷冻球囊的肺静脉隔离(CB-PVI)已被广泛用于治疗心房颤动。虽然该操作一般安全有效,但该操作可能与肺静脉狭窄和支气管或食管损伤有关。导致这些并发症的机制尚未详细研究。近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员的目的是评估球囊对肺血管和右心压力以及肺静脉壁形态的急性影响。
在8例接受了CB-PVI的患者(5名男性,平均年龄为55±14岁)中,导管位于肺静脉内在CB-PVI前后直接测量每个肺静脉的压力。同时也测量了右心房、右心室、肺动脉压和肺动脉分支中的肺动脉楔压。应用血管内超声评价肺静脉的形态学改变。
研究人员发现消融前后肺静脉内压力无显著差异。在冷冻法期间肺动脉毛细血管楔压明显升高(左上:20±10 vs. 29±8.5mmHg,P=0.004;左下:24±10 vs. 32±6mmHg,P=0.012;右上:25±9 vs. 35±10 mmHg,P=0.002;右下:24±10 vs. 37±12mmHg,P=0.0036)。CB-PVI后右心房和肺动脉压力显著增加(9±6 vs. 13±8mmHg,P=0.004,以及20±9 vs. 24±10mmHg,P=0.048)。血管内超声显示90%的急性水肿和夹层样改变导致肺静脉管腔相对变窄90%。
由此可见,CB-PVI操作导致肺动脉和右心房压力显著上升,以及导致肺静脉壁损伤。这些研究结果的临床意义值得进一步研究。
原始出处:
Jakub Baran,et al. Acute Hemodynamic and Tissue Effects of Cryoballoon Ablation on Pulmonary Vessels: The IVUS‐Cryo Study.JAHA.2017. https://doi.org/10.1161/JAHA.117.005988
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#血流动力#
88
#AHA#
88
#球囊#
91
#血流动力学#
75
#消融#
86
学习了,感谢分享。
99