德国科学家日前发表的一项医学研究成果显示,肥大细胞增生症引起的严重病变,可以通过靶向药物米哚妥林得到缓解。
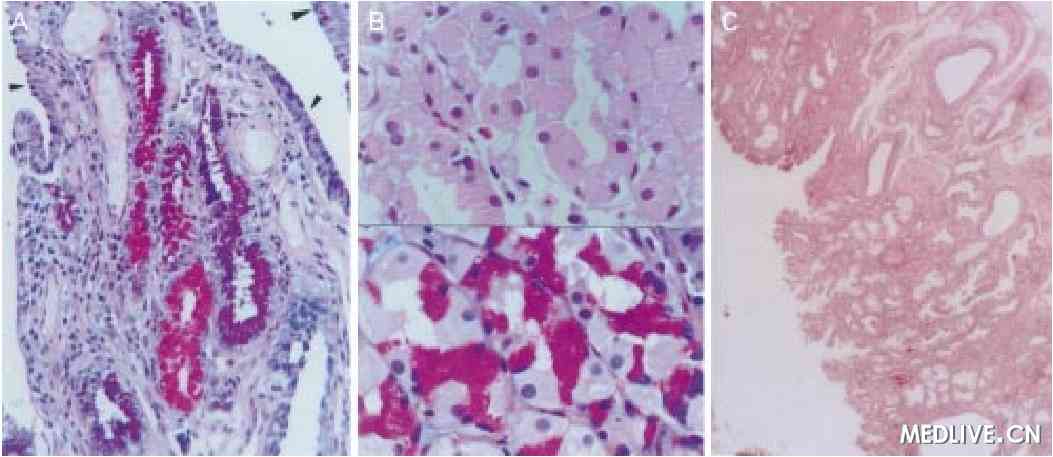
肥大细胞增生症是一种目前病因尚不完全明确的罕见疾病,特点是肥大细胞通过浸润性增生侵入周围组织,一般被认为与原癌基因KIT的激活性突变有关,这种基因的产物是Ⅲ型酪氨酸激酶。罹患此病后,病人会出现过敏、皮肤病变、体重下降和贫血等症状,严重时可转化为白血病。
最新研究覆盖了超过100名患有严重肥大细胞增生症的病人,是相关领域迄今规模最大的研究。研究人员发现,一种名为Midostaurin(米哚妥林)(PKC412)的酪氨酸激酶抑制剂,能够有选择性地抑制激活性突变KIT基因,通过这一靶向药物治疗,参与研究的约六成严重患者病情得到明显好转。
这项发表在美国《新英格兰医学杂志》上的研究显示,米哚妥林能遏制器质性病变和肥大细胞的浸润性增生,患者寿命能由此平均延长28.7个月。
原始出处
Jason Gotlib, M.D., Hanneke C. Kluin-Nelemans, M.D., Ph.D., Tracy I. George, M.D., Cem Akin, M.D., Ph.D., Karl Sotlar, M.D., Olivier Hermine, M.D., Ph.D., Farrukh T. Awan, M.D., Elizabeth Hexner, M.D., Michael J. Mauro, M.D., David W. Sternberg, M.D., Ph.D., Matthieu Villeneuve, M.Sc., Alice Huntsman Labed, Ph.D., Eric J. Stanek, Pharm.D., Karin Hartmann, M.D., Hans-Peter Horny, M.D., Peter Valent, M.D., and Andreas Reiter, M.D.Efficacy and Safety of Midostaurin in Advanced Systemic Mastocytosis.NEJM.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#IDO#
79
好文章,受益
91
赞一个!好文章拜读了,认真学习了。
1
学习了,好
86
#Tau#
75
#肥大细胞#
77