Clin Gastroenterology H:英夫利昔单抗的累积暴露量而非谷浓度与感染率相关
2021-01-18 MedSci原创 MedSci原创
虽然TNF拮抗剂英夫利西单抗在治疗炎症性肠病(IBD)中疗效比较受到公认,但仍然存在一些严重的不良事件的发生,尤其是感染和恶性肿瘤。
虽然TNF拮抗剂——英夫利西单抗在治疗炎症性肠病(IBD)中疗效比较受到公认,但仍然存在一些严重的不良事件的发生,尤其是感染和恶性肿瘤的发生。有研究显示克罗恩病患者(CD)接受英夫利西单抗治疗后严重感染的风险增加,而英夫利西单抗药物暴露程度和这种风险被怀疑存在相关性。英夫利西单抗的药物谷浓度(TLI) 水平被认为是影响患者感染的最关键的因素。但是有文献认为总体的累计暴露量与感染有关系。因此,本项研究旨在探究英夫利昔单抗治疗的患者感染相关的因素,包括药代动力学特征。

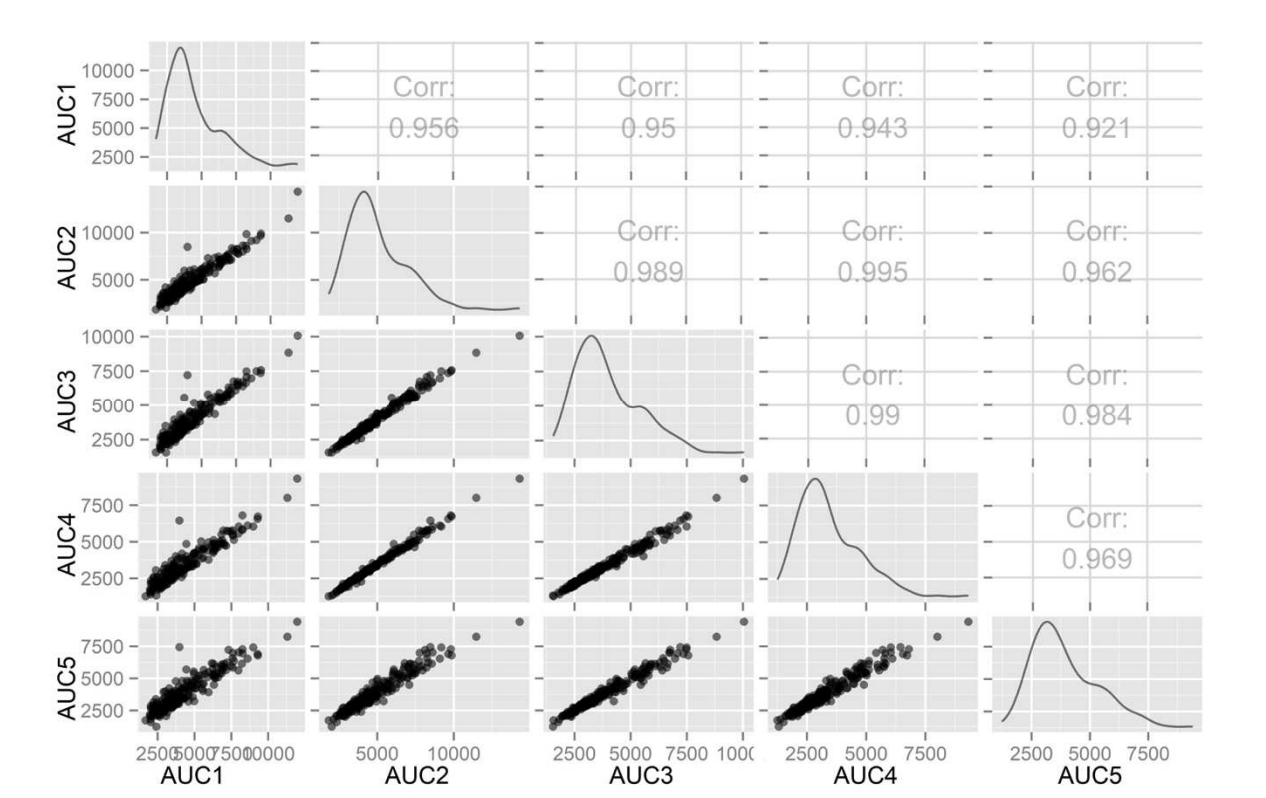
研究人员收集了2016年11月至2017年4月间在法国接受英夫利昔单抗维持治疗的209例IBD患者的临床上数据(其中159克罗恩病; 54例接受药物联合治疗)。英夫利昔单抗的暴露是根据药代动力学模型中药物浓度的曲线下面积(AUC)估算的。根据AUC的总和估算6个月内的个人总暴露量。
研究结果显示英夫利昔单抗谷浓度平均水平为5.46 mg / L,累计AUC的平均水平为3938±1427 mg.d / L。从640次输液访问中总共收集到215次感染的现象发生;123名患者(59%)至少感染1次。经过多变量分析后,与感染独立相关的因素包括吸烟(优势比[OR],2.05; P = .046),IBD复发(OR,2.71; P = .006)和英夫利昔单抗的累计ΣAUC高(3234 mg.d / L)(OR,2.02; P = .02)。发生感染的患者中的ΣAUC较高( P = .04),并且与感染次数相关(P = .04)。英夫利昔单抗的低谷浓度与感染无关。
因此,通过本项研究研究人员证实:英夫利昔单抗治疗的患者中有近三分之二发生了感染。感染风险与药物暴露的累积增加相关,但与英夫利昔单药谷水平无关。
原始出处 :
Amandine Landemaine. Et al. Cumulative Exposure to Infliximab, But Not Trough Concentrations, Correlates With Rate of Infection. Clin Gastroenterology H.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Gastroenterol#
41
#AST#
41
#GAS#
66
#Gastroenterology#
57
#浓度#
43