Nature :新型化合物可以降低乳腺癌症的转移
2017-03-14 Rongrong 药渡头条
所有成功的新一代对抗癌症的免疫疗法,经常是未能作用于免疫系统的所有分支。这种治疗方法作用于自适应性的免疫系统,对外来细胞和患病细胞进行准确攻击。免疫系统的另一分支,被称为天然免疫,在整个免疫过程中可能不只是闲置着,实际上有可能促使肿瘤的生长。Dana-Farber 癌症研究所的研究人员近日在《Nature》杂志上发表了一项新的研究成果。一种化合物能够扭转先天免疫系统细胞的忠诚——把他们从肿瘤的推动
所有成功的新一代对抗癌症的免疫疗法,经常是未能作用于免疫系统的所有分支。这种治疗方法作用于自适应性的免疫系统,对外来细胞和患病细胞进行准确攻击。免疫系统的另一分支,被称为天然免疫,在整个免疫过程中可能不只是闲置着,实际上有可能促使肿瘤的生长。
Dana-Farber 癌症研究所的研究人员近日在《Nature》杂志上发表了一项新的研究成果。一种化合物能够扭转先天免疫系统细胞的忠诚——把他们从肿瘤的推动者变成肿瘤的对抗者——使得小鼠乳腺肿瘤缩小并不再转移。当联合化疗或者其他免疫治疗期间,新化合物显着延缓了肿瘤的生长时间。作者表示,该研究发现了一种新的方法用来全面激活免疫系统来对抗癌症。
“最新形式的癌症免疫治疗方法影响 T 细胞的行为——白细胞是适应性免疫系统的一部分——“教”它们攻击肿瘤细胞或者消除这种攻击障碍”,这项研究的主要作者 Jennifeer Guerrier 解释到,“这种策略对几种类型的癌症都有疗效,但是通常只有一小部分的患者受益。我们想知道如果利用免疫系统的两个方面作用是否可以产生更卓越的结果。”
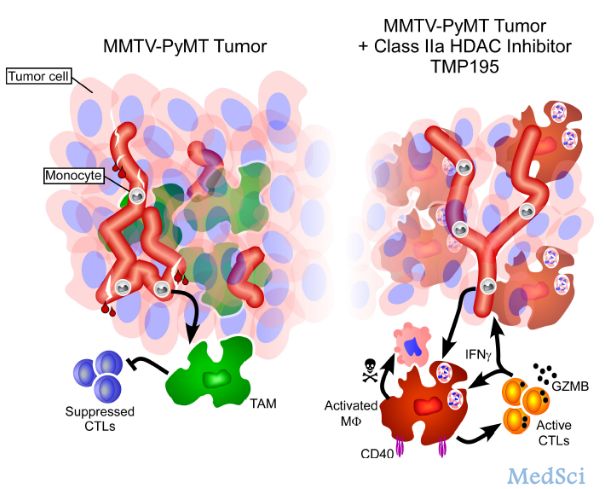
这项新研究的靶标是被称为肿瘤相关巨噬细胞 (TAMs) 的先天免疫系统细胞。它们经常被发现深深嵌入在肿瘤中,尽管它们是身体防御疾病的免疫系统的一部分——但是它们经常促进肿瘤的生长。在这一过程中,它们对肿瘤发出的信号也产生响应。
巨噬细胞扮演的角色——无论是保护或者破坏性的——取决于它们所处环境所发出的信号。例如,在伤口愈合中,巨噬细胞集结免疫系统元素清除受损组织,恢复受影响的区域。而肿瘤巨噬细胞为了自身目的劫持了部分支持功能,所以,癌症有时被称为不会愈合的伤口也不是没有道理的。
在之前的研究中,dana-farber 研究所的研究人员发现,一种被称为 TMP195 的化合物可以将 TAM 从协助肿瘤生长转变成对抗肿瘤生长。TMP195 一个选择性的,最新型的,IIa HDAC 抑制剂,通过在 TAMs 中改变基因功能从而转变巨噬细胞的反应。
在这次研究中,研究人员发现 TMP195 大幅度降低了小鼠乳腺肿瘤的肿瘤生长率。接下来,研究人员将 TMP195 与不同的化疗方案或者一种被称为 T 细胞免疫检查点阻断的免疫疗法相结合。在这两种情况下,联合用药比单独使用 TMP195 能更持久的缓解乳腺癌生长速度。
“一旦发生转换,巨噬细胞就成为免疫系统攻击肿瘤的协助者” Dana-Farber 研究所的资深作者医学博士 Anthony Letai 说“我们的研究证明 IIa HDAC 抑制剂可以有效的开发巨噬细胞的抗肿瘤潜力。”
“癌症治疗的未来可能涉及到作用于先天免疫和适应性免疫系统的组合疗法,以及作用于癌症本身的其他疗法,例如化疗,放射治疗,或者靶向治疗,”。Anthony Letai 表示,“能够让先天免疫系统加入到对癌症的治疗方案中,是一个令人兴奋的新方向。”
原始出处:
Jennifer L. Guerriero,Alaba Sotayo,Holly E. Ponichtera,et al.Class IIa HDAC inhibition reduces breast tumours and metastases through anti-tumour macrophages, Nature (2017) doi:10.1038/nature21409
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#化合物#
0
#Nat#
62
值得学习
92
值得学习
98