Eur Heart J:外周动脉疾病患者经血管内和手术血运重建的长期结局比较
2021-02-25 MedSci原创 MedSci原创
尽管两种治疗策略的长期MALE风险相当,但经手术血管重建具有降低长期死亡率的优势。
外周动脉疾病(PAD)可通过血管内治疗或开放手术的方法进行血运重建。尽管通过血管内治疗进行血运重建术的患者有所增加,但仍不确定哪种治疗策略能够获得更好的长期结局。
近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,该回顾性队列研究评估了澳大利亚和新西兰住院的PAD患者,这些患者在2008年至2015年间接受了血管内血运重建术或外科手术治疗。研究人员使用倾向得分匹配分析进行了比较。研究人员排除了混合干预。该研究的主要终点是死亡或严重不良肢体事件(MALE),定义为住院后长达8年的急性肢体缺血、紧急外科手术或血管内再干预或重大截肢的复合终点。研究人员采用时间-事件分析了75189名 符合条件的患者(15239例手术患者和59950名血管内治疗患者),并从中确定了14339对配对患者(年龄均值±SD为71±12岁,男性占73%),且协变量平衡良好。
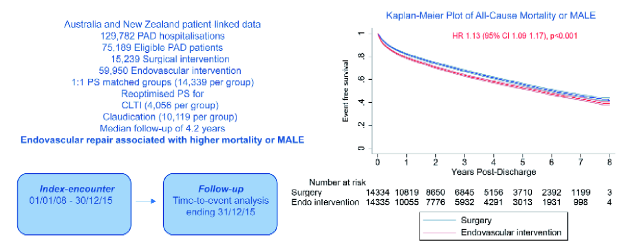
研究人员发现血管内治疗血运重建与合并的MALE或死亡率增加相关[风险比(HR)为1.13,95%置信区间(CI):1.09-1.17,P<0.001]。当血管内治疗与手术治疗相比,MALE(HR为1.04,95%CI:0.99-1.10,P=0.15)和全因紧急住院治疗(HR为1.01,95%CI:0.98-1.04,P=0.57)的风险相似,但死亡率较高(HR为1.16,95%CI:1.11-1.21,P<0.001)。在亚组分析中,这些发现与间歇性跛行和长期肢体缺血的临床表现均一致。
由此可见,尽管两种治疗策略的长期MALE风险相当,但经手术血管重建具有降低长期死亡率的优势。这与以前的PAD研究不一致,进一步凸显了这一领域存在的争议。
原始出处:
Saman L Parvar,et al.Long-term outcomes following endovascular and surgical revascularization for peripheral artery disease: a propensity score-matched analysis.European Heart Journal.2021.https://doi.org/10.1093/eurheartj/ehab116
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#疾病患者#
80
哈哈哈哈哈哈哈
103
学习
129
#ART#
76
#长期结局#
80
#HEART#
67
#外周动脉#
62
有争议,但还是觉得手术开放治疗更好
124
外周动脉疾病(PAD)可通过血管内治疗或开放手术的方法进行血运重建。
113