Cell:重磅!首次揭示大脑血清素系统至少由两组血清素能神经元亚群组成
2018-08-29 佚名 细胞
化学信使分子血清素(serotonin,也称作5-羟色胺)与从情绪到运动调节的一切相关。但是迄今为止,人们还远未明确血清素对哺乳动物大脑的影响。科学家们给出了不同的结果。一些人发现血清素能促进快乐。另一些发现它增加焦虑的同时抑制运动,而其他人持相反的观点。
在一项新的研究中,来自美国斯坦福大学的Liqun Luo教授及其团队着重关注脑干中的一个被称作中缝背核(dorsal raphe)的区域,这个区域含有哺乳动物大脑中最大密度的都通过释放血清素传递信号的神经元(大约9000个)。相关研究结果于2018年8月23日在线发表Cell期刊上,论文标题为“Anatomically Defined and Functionally Distinct Dorsal Raphe Serotonin Sub-systems”。
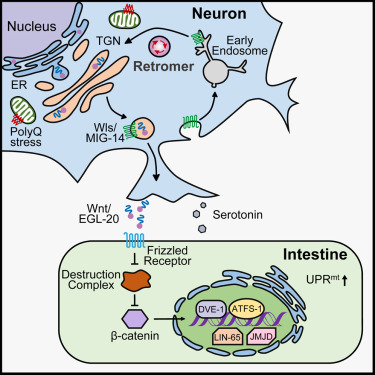
这些中缝背核神经元的神经纤维或者说轴突与很多至关重要的执行着一系列功能(包括思考、记忆、情绪和身体功能的调节)的前脑区域形成一个庞大的连接网络。通过注射感染这些区域中的血清素轴突(serotonin axon, 注:血清素能神经元的轴突)的病毒,这些研究人员能够将这些连接追溯到它们在中缝背侧中的原始神经元。
这允许他们构建出脑干中致密的血清素释放神经元(serotonin-releasing neuron, 也称作serotonin neuron,即血清素能神经元)到它们影响的多个前脑区域的神经投射的视觉图谱。这种图谱揭示出在中缝背核中至少存在着两组不同的血清素能神经元,它们与大脑中的皮层和皮层下区域相连。
在一系列行为测试中,这些研究人员还证实这两组血清素能神经元对刺激作出不同的反应。比如,当小鼠接受到喝糖水之类的奖励时,这两组血清素能神经元都会放电,但是它们对轻度的足部电击等惩罚作出相反的反应。
Luo说,“我们如今明白为何一些科学家们认为血清素能神经元被惩罚激活,而另一些人认为它们被惩罚抑制。这两种说法都是对的---它仅取决于你研究哪组血清素能神经元。”
更重要的是,这些研究人员发现血清素能神经元本身比之前想象的更加复杂。投射到皮层区域的血清素能神经元并不仅仅利用血清素传递信息,还会释放出一种叫做谷氨酸的化学信使,这让它们成为大脑中释放两种不同化学物质的少数神经元之一。这就产生一个问题,即人们是否应当称呼它们为血清素能神经元,毕竟神经元是根据它们释放的神经递质命名的。
总之,这些研究结果表明,大脑的血清素系统不是由同质的神经元群组成,而是由许多协同发挥作用的神经元亚群(或者说子系统)组成。Luo团队鉴定出两组神经元亚群,但可能存在着更多组的神经元亚群。
事实上,斯坦福大学医学院精神病学与行为科学教授Robert Malenka及其团队最近在中缝背核中发现了一组投射到伏隔核(nucleus accumbens)的血清素能神经元。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Cell#
80
#CEL#
74
#血清素系统#
103
#重磅#
85
学习了
126