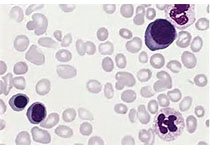
Blood:消化道抗原提呈细胞在alloHSCT后GVHD中的重要作用
2019-11-05 QQY MedSci原创
同种异体干细胞移植仍然是治疗高危和/或晚期血液系统恶性肿瘤的基础,但仍受到移植物抗宿主病(GVHD)的限制。GVHD是由受体抗原提呈细胞(APC)与供体T细胞相互作用而引起的,T细胞分化成1型(Th1/Tc1)和17型(Th17/Tc17)致病性T细胞,导致抗原耐受性调节T细胞(Treg/Tr1)模式被破坏。1型和17型T细胞分泌对细胞因子风暴至关重要的细胞因子(如GM-CSF和IFNg),增强供
GVHD是由受体抗原提呈细胞(APC)与供体T细胞相互作用而引起的,T细胞分化成1型(Th1/Tc1)和17型(Th17/Tc17)致病性T细胞,导致抗原耐受性调节T细胞(Treg/Tr1)模式被破坏。1型和17型T细胞分泌对细胞因子风暴至关重要的细胞因子(如GM-CSF和IFNg),增强供体APC扩增极其同种抗原提呈。
在移植前后,这些APC会受到来自调节和肠道微生物群的PAMP/DAMP信号的明显影响。随后,消化道的供体DC会被结肠中的DAMP/PAMP信号激活,一旦粘膜屏障被GVHD破坏,这些信号就会到达固有层。从而导致结肠中的供体DC扩增和同种抗原提呈,随后迁移至肠系膜淋巴结。在这里,新的供体T细胞被启动、扩增、分化,并被烙上允许迁移到受损胃肠道的内脏归巢整合素印迹,最终导致发生致死性的GVHD前馈级联反应。
本文有助于引发我们对启动GVHD的细胞和分子因子的新见解,从而发现许多合理的治疗靶点,此外,本文还强调了抑制消化道APC功能的重要性。
原始出处:
Geoffrey R. Hill, et al.The primacy of gastrointestinal tract antigen presenting cells in lethal graft-versus-host disease.Blood. 2019,November 04.
本文系梅斯医学(MedSci)原创编译,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#HSC#
86
#重要作用#
60
#ALL#
73
#消化道#
108
#HSCT#
82
#抗原#
111