Laryngoscope:口腔卫生差,警惕涎石病的发生
2016-02-10 MedSci MedSci原创
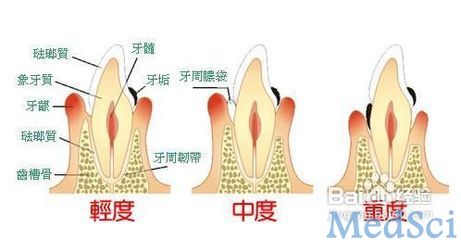
Laryngoscope:口腔卫生差,警惕涎石病的发生尽管普遍认为较差的口腔卫生可导致涎石病的发展,但是却鲜有研究支持此观点。因此,本研究旨在基于覆盖全国的数据库评估慢性牙周炎和日后唾液腺结石发生之间的关系。研究采用病例对照研究。共纳入987名涎石病患者。再按5:1(健康者:患者)的比例纳入4935名健康者,匹配性别和年龄。使用条件Logistic回归分析确定涎石病与慢性牙周炎之间的关系。结果发现
尽管普遍认为较差的口腔卫生可导致涎石病的发展,但是却鲜有研究支持此观点。因此,本研究旨在基于覆盖全国的数据库评估慢性牙周炎和日后唾液腺结石发生之间的关系。
研究采用病例对照研究。共纳入987名涎石病患者。再按5:1(健康者:患者)的比例纳入4935名健康者,匹配性别和年龄。使用条件Logistic回归分析确定涎石病与慢性牙周炎之间的关系。
结果发现,5922名研究对象中共有1831名既往曾诊断为慢性牙周炎。卡方检验显示,病例组和对照组之间既往慢性牙周炎的患病率存在显著的差异(36.8% vs. 29.7%,P<0.001 )。校正地理位置和烟草的使用后,条件Logistic回归分析显示,与对照组相比,病例组既往慢性牙周炎的比值比为1.37(95% CI为1.19-1.56)。进一步分析既往慢性牙周炎与涎石病之间的关系与性别的关联,发现既往慢性牙周炎与涎石病的关系不受性别的影响。与对照组相比,病例组男性既往慢性牙周炎校正后的比值比为1.34(95% CI为1.10-1.64),女性为1.41(95% CI为1.15-1.73)。
总而言之,该研究表明,慢性牙周炎与涎石病的发生之间存在关联。
Hung SH, Huang HM, Lee HC, Ching Lin H, Kao LT, Wu CS. A population-based study on the association between chronic periodontitis and sialolithiasis. Laryngoscope. 2016 Jan 25. doi: 10.1002/lary.25360.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PE#
54
好文章,还会关注
82
赞了!深度好文,深入学习。
96
#口腔卫生#
84
学习!
149
注意口腔卫生
183