European Radiology:T2*mapping在显示膝骨关节炎患者早期半月板异常中的价值
2022-06-11 shaosai MedSci原创
传统的MRI虽然是揭示半月板异质性的最有价值的影像学方法,对临床诊断和治疗也有很大帮助,但由于半月板高度胶原结构中水的T2时间很短(在1.5T下约5-8ms),可能会导致T2的高估。

众所周知,半月板在稳定和维持膝关节的正常功能方面起着重要作用。半月板损伤或退变可能与软骨体积损失、骨髓病变或膝关节创伤后软骨下骨灌注的改变有关。使用磁共振成像(MRI)确定的半月板损伤程度,可与膝关节疼痛的严重程度相关。尽管半月板受累的病理机制和随后的膝关节OA的发展仍不明确,但对膝关节半月板损伤和OA之间关系的研究已得到越来越多的关注,这表明在OA发展过程中观察半月板的基础结构变化的重要性。
一些定量的MR测量,包括延迟钆(Gd)增强的MRI、T1 rho和T2mapping已被开发出来用以揭示膝关节半月板在病理严重程度的不同阶段或OA进展期间的基础结构信息。虽然退化的半月板中糖胺多糖和蛋白多糖浓度的变化可能与T1和T1 rho弛豫时间的改变有关,但MR T2测量在临床应用中更有价值。据报道,T2值反映了膝关节半月板中水含量和胶原纤维方向的细微变化,这些指标都是提示半月板退化的信号,并与OA的严重程度相关。
传统的MRI虽然是揭示半月板异质性的最有价值的影像学方法,对临床诊断和治疗也有很大帮助,但由于半月板高度胶原结构中水的T2时间很短(在1.5T下约5-8ms),可能会导致T2的高估。最近的研究已证明了三维超短回波时间(UTE)成像序列在揭示尸体半月板的微观结构方面的能力。然而,三维成像的不均匀层厚和较长的采集时间会限制其临床应用。
近日,发表在European Radiology杂志的一项研究验证了二维径向T2*mapping在OA患者中检测早期半月板异常的可行性,为半月板病变的早期识别及诊断提供了技术支持。
本研究纳入了40名参与者,其中20人被诊断为OA,20人是年龄和性别匹配的无症状对照。使用配有单通道膝关节线圈的1.5T磁共振成像收集每个参与者的右膝数据。使用传统的T2*mapping方案和径向T2*mapping方法获得T2*值。计算了半月板白区、半月板红区和整个半月板的平均T2*值,并进行了数字模拟验证。
模拟和临床数据都证实,二维径向T2*mapping提供了比传统方法更好的辨别能力。与对照组相比,OA组在白区(9.33 [2.29] ms vs. 6.04 [1.05] ms)、红区(9.18 [2.03] ms vs. 6.81 [1.28] ms)和总半月板(9.26 [2.06] ms vs. 6.34 [1.14] ms)的T2*值中都显示出明显更好的平均值(标准偏差)。所有三个区域的Lequesne指数和半月板T2*值之间都有相关性(分别为r = 0.528,p = 0.017;r = 0.635,p = 0.003;r = 0.556,p = 0.011)。
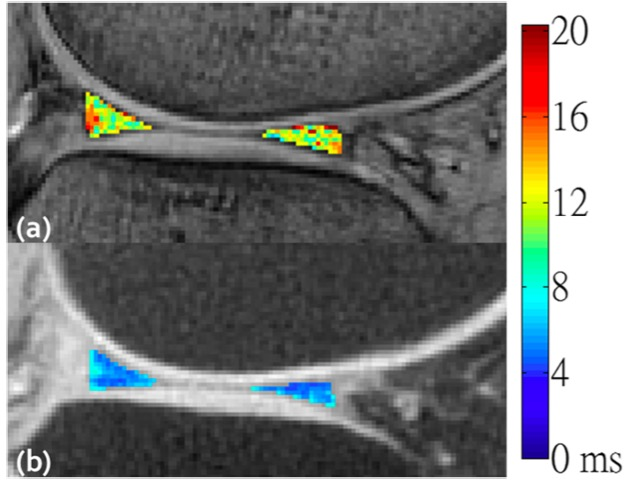
图 对于无症状的对照组样本,由常规T2*mapping(a)和径向T2*mapping(b)得出的T2*mapping
本研究表明,与传统的T2*mapping相比,二维径向T2*mapping在检测早期半月板退化方面更有优势,这一点已被临床评估所证实。这些发现表明,该技术提供了一种替代手段来揭示早期OA中膝关节半月板的基础结构变化,并在临床应用中具有诊断潜力。
原文出处:
Ping-Huei Tsai,Chin-Chean Wong,Wing P Chan.Radial T2* mapping reveals early meniscal abnormalities in patients with knee osteoarthritis.DOI:10.1007/s00330-022-08641-6
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#mapping#
79
#膝骨#
64
#骨关节#
76
#PE#
56
#关节炎#
67
#膝骨关节炎#
101
#半月板#
87