实验性药物3K3A-APC用于急性缺血性卒中的治疗
2018-02-28 MedSci MedSci原创
近日,初步的II期临床试验数据表明,急性缺血性中风患者对高剂量3K3A-APC耐受,试验结果还显示3K3A-APC可显著减少患者的出血量和出血发生率,因此这是一种有前途的抗中风药物。
近日,初步的II期临床试验数据表明,急性缺血性中风患者对高剂量3K3A-APC耐受,试验结果还显示3K3A-APC可显著减少患者的出血量和出血发生率,因此这是一种有前途的抗中风药物。
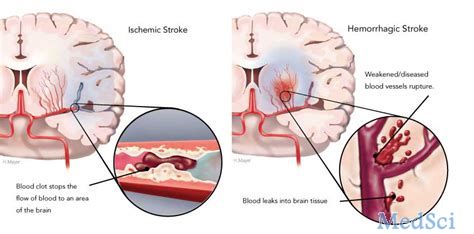
“这些结果为接下来获得FDA的批准奠定了基础,” Scripps研究所的John Griffin教授说。中风是美国第五大死因,也是成年残疾的头号原因。急性缺血性中风发生在血块阻塞血液流向大脑时。 迄今为止,FDA已批准仅一种称为组织纤溶酶原激活剂(tPA)的药物治疗来治疗急性缺血性中风,如果在中风后的4.5小时内给药,tPA有助于分解血块。但不幸的是,由于这个极短的治疗窗口以及它可能导致大脑出血和神经元细胞死亡的副作用,导致了tPA的使用受到限制。 迄今为止的研究表明3K3A-APC可以有效补充tPA的作用。 John Griffin教授通过修改血液蛋白C的三种氨基酸来设计实验药物,值得注意的是该蛋白既是抗凝血剂又是细胞保护剂。
原始出处:
https://www.europeanpharmaceuticalreview.com/news/73025/3k3a-apc-ischemic-stroke/
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#缺血性#
53
#实验性#
55
#缺血性卒#
70
#APC#
72