【所属科室】
呼吸科
【基本资料】
男,80岁
【主诉】
查体发现右上方占位2周
【现病史】
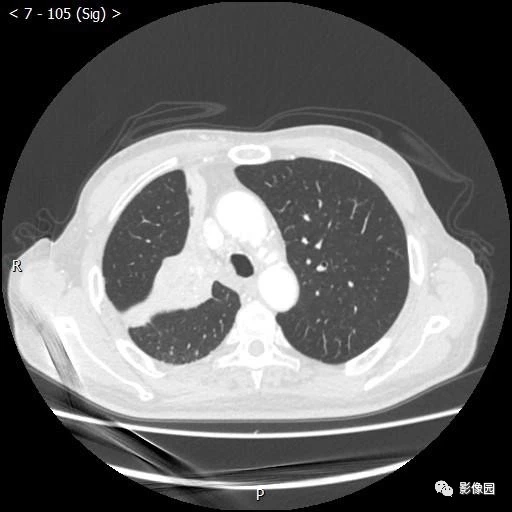
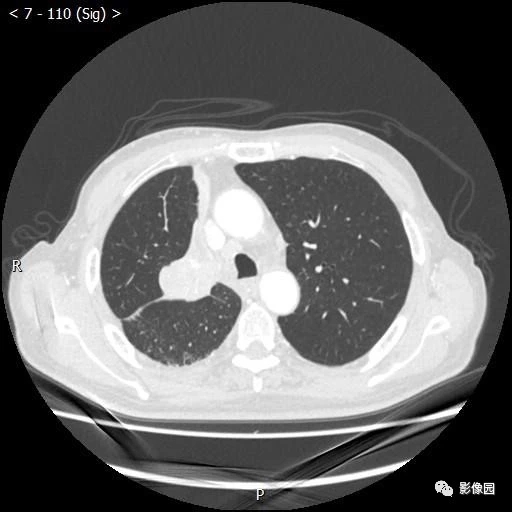
患者近期由于消瘦于当地医院查体发现右上肺占位,患者偶有咳嗽咳痰,无明显胸闷气短,就诊于当地医院查胸部CT提示右上肺病变。
【影像图片】




【讨论问题】
诊断?
【医学影像APP用户讨论】
评论:右肺上叶、中叶不张,病变与肺组织分界不清,右肺上叶支气管闭塞,右主支气管、右肺中叶、下叶支气管狭窄。
考虑中央型肺癌,累及上叶、中叶支气管。
【结果】
(气管镜活检,右上肺肿物)中分化鳞状细胞癌。
【病例小结】
中央型肺癌发生在主支气管、肺叶支气管和肺段支气管。生长类型可分成管外型、管壁型、管内型,其中以管外型为主,以腺癌、鳞癌等为主要病理类型。肿瘤的病理形态包括支气管管壁增厚、管腔内肿物和支气管周围肿块。肿瘤的生长使支气管狭窄或阻塞,可引起阻塞性肺气肿、阻塞性肺炎及阻塞性肺不张,即所谓三阻征象。
X线特征如下:
1 早期X线检查不存在异常表现。
2 伴随患者病情进展,肺门部位可见突向肺野、边缘清晰的肿块影。3 肿瘤组织若阻塞气管可产生典型“三阻征”影像学表现,即阻塞性肺气肿、阻塞性肺炎、阻塞性肺不张,其中以阻塞性肺不张最为常见。阻塞性肺炎——肿瘤阻塞气道时,相应肺段、肺叶区域有模糊索条状片状或索条状影,密度均匀。阻塞性肺气肿——若肺叶体积明显增大,肺纹理较稀疏,透明度较高,横膈、纵膈可受压而移位。肺不张——若气管彻底阻塞,可产生片状肺不张阴影。
4 伴发肺门淋巴结肿大,其下缘有倒“S”状影,即中央型肺癌,是右上叶中央型肺癌典型征象。
CT特征如下:
1 早期CT检查可见其管壁有轻度增厚情况,且管腔中有小结节、管腔阻塞或狭窄;中期、晚期的中央型肺癌患者直接征象为支气管阻塞、狭窄、肺门肿块,以支气管狭窄最为明显,表现为管腔内缘光滑或者不规则,管壁增厚;其中,支气管阻塞的主要表现为管腔变细后阻塞,管腔骤然截断;肺门肿块的主要CT表现为肺门区域外缘光滑,或者出现分叶状软组织肿块影:中央型肺癌间接征象是肿瘤未完全梗阻支气管时所致阻塞性肺气肿,肿瘤彻底阻塞支气管时,其相应部位有阻塞性肺不张、阻塞性肺炎等表现,CT表现为斑片状的模糊影,或者肺叶、肺段实变影;增强扫描后,在明显强化不张肺叶的衬托下,其狭窄支气管会显示的更清楚。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#中央型#
90
#中央型肺癌#
86
学习了.谢谢分享
111
学习了
125