


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



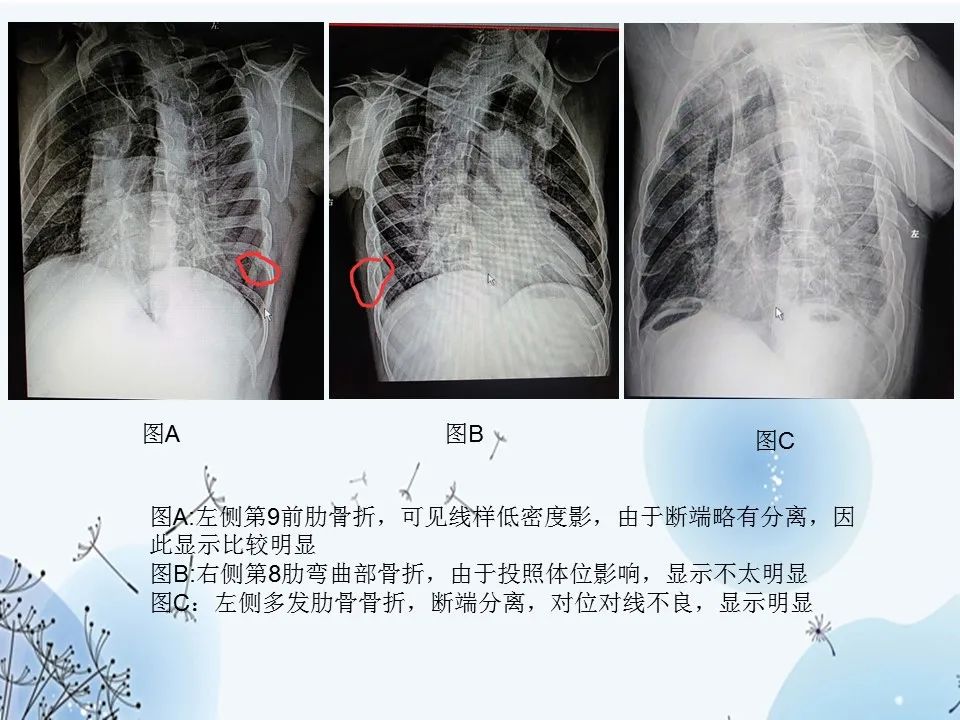
肋骨骨折是钝性胸部外伤中最常见的创伤形式,发生于约50%的患者。诊断肋骨骨折的常规影像学检查是胸部X线平片。但是,这种方式的灵敏度较低,仅为15%。
肋骨骨折是外伤患者中常见的损伤,老年肋骨骨折患者发生不良事件和死亡的风险增加。近日,一项单中心、随机、安慰剂对照、双盲的研究旨在确定口服对乙酰氨基酚(PO)在治疗与肋骨骨折相关的疼痛方面是否与静脉注射
国际上,胸部X线检查是怀疑婴儿身体受虐待时检查肋骨骨折的标准方法。几个针对儿童的小观察性研究发现对于骨折,胸部CT的准确率要高于X线检查;但是,据了解,该准确性尚未得到全面评估。现研究人员对尸检后胸片和胸部CT肋骨骨折检出率的差异进行对比,以法医尸检为参考标准。研究人员开展一回顾性的诊断准确性研究,对2012年1月1日-2017年1月1日期间在英国伦敦大奥蒙德街医院进行死亡调查的所有采取验尸骨骼检
女子出车祸后被送到医院治疗,医院没有发现女子右侧多根肋骨骨折,半个多月后,女子病情严重不幸去世。法医鉴定,女子因外伤致右侧第4-6肋骨骨折、创伤性湿肺继发肺内感染、致呼吸功能衰竭死亡。经鉴定,大连两家医院在女子诊疗过程中存在过错,法院判决两家医院赔偿死者家属30多万元。女子骨折遭医院漏诊2017年1月1日13时50分左右,高女士乘坐的轿车与一辆货车相撞,高女士受伤,随后被120送到旅顺A医院救治,
2019年5月,美国放射学会(ACR)发布了肋骨骨折的影像学检查标准指导,肋骨骨折是轻微钝挫伤后最常见的胸部损伤,本文主要针对肋骨骨折恰当影像学检查提出指导建议,涉及胸部X线检查,CT检查以及Tc-99m骨扫描检查。
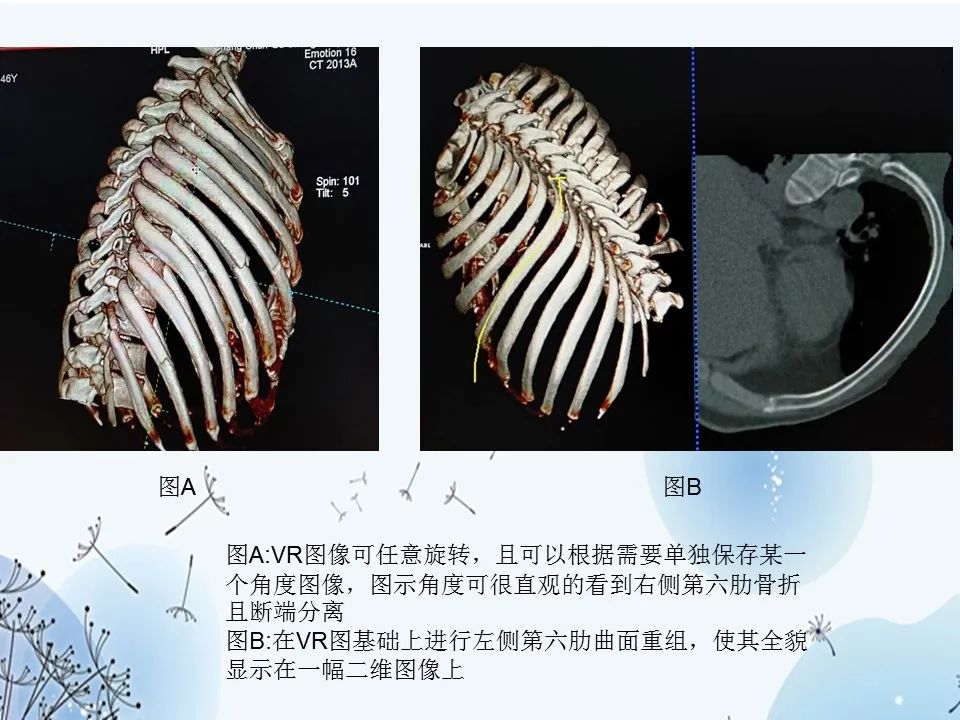
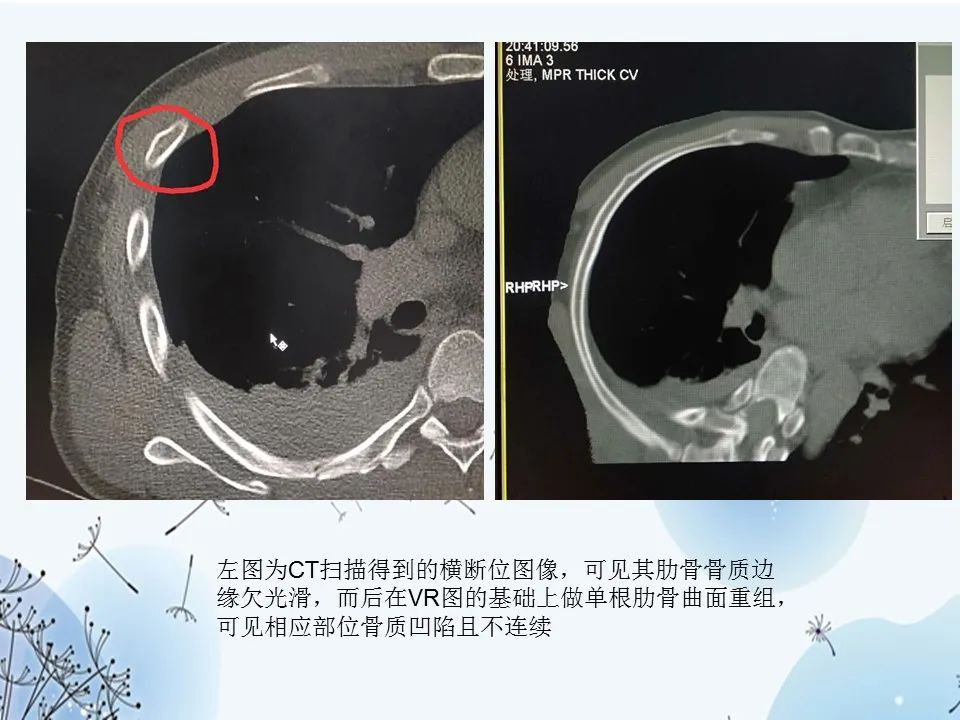
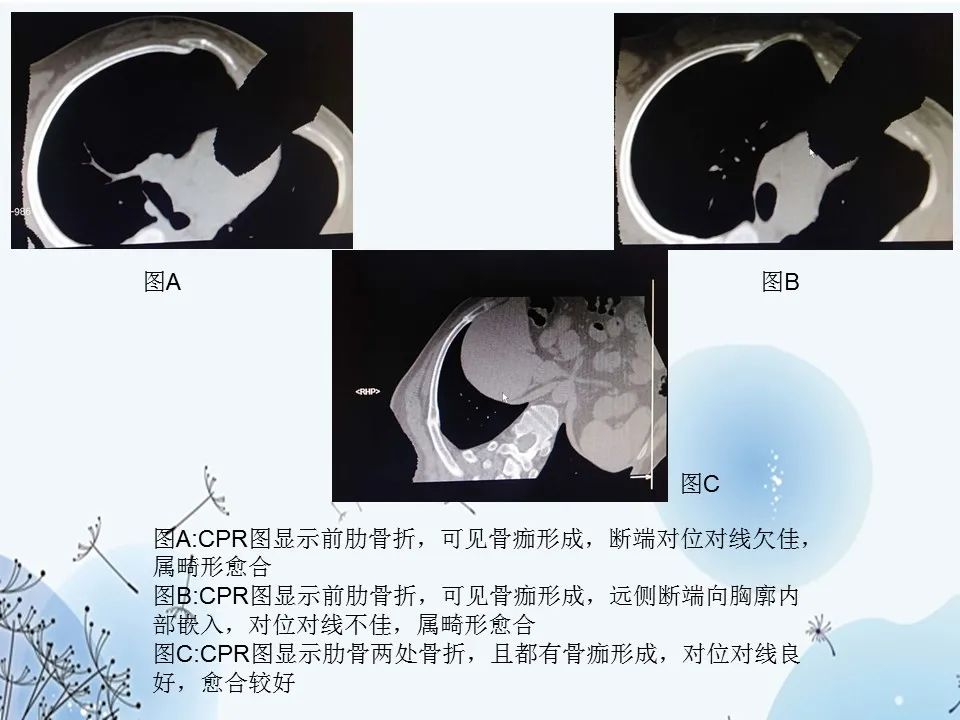
放射科医师的眼是保住工作的铁饭碗,然而,有些工作偏偏想砸了他的铁饭碗!


梅斯医学MedSci APP
医路相伴,成就大医
#联合应用#
69
#CPR#
89
#评价#
56
#肋骨骨折#
78
!!
87
或病人有胸痛时,立即停药及时
108
学习
119