JBC:癌细胞内组蛋白mH2A1.2与HER-2之间相互作用的机制
2012-05-19 Deepblue 生物谷
原癌基因人类表皮生长因子受体2(HER-2)一般在癌细胞内过量表达,但是其机制目前仍不明确。近日,来自夏威夷大学的研究人员Scott K. Kuwada等人表示,癌细胞内非典型组蛋白macroH2A1.2与HER-2的相互作用能够促进原癌基因的表达及细胞增生。 研究发现,在HER-2过表达的癌细胞内,非典型组蛋白macroH2A1能够与HER-2相互作用。人类mH2A1具有两种亚型,mH2A1.

原癌基因人类表皮生长因子受体2(HER-2)一般在癌细胞内过量表达,但是其机制目前仍不明确。近日,来自夏威夷大学的研究人员Scott K. Kuwada等人表示,癌细胞内非典型组蛋白macroH2A1.2与HER-2的相互作用能够促进原癌基因的表达及细胞增生。
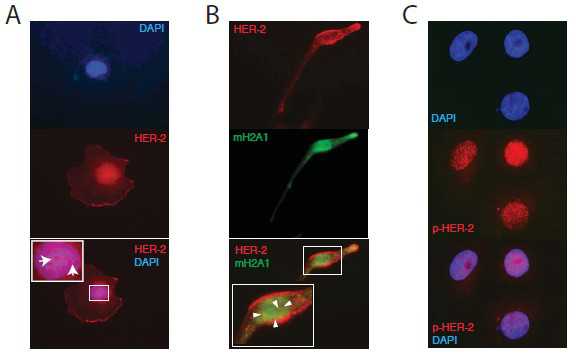
研究发现,在HER-2过表达的癌细胞内,非典型组蛋白macroH2A1能够与HER-2相互作用。人类mH2A1具有两种亚型,mH2A1.2与mH2A1.1。在人癌细胞系,他们发现mH2A1.2而不是mH2A1.1,能够与HER-2相互作用。
在致瘤性及HER-2表达显著提高的癌细胞,他们发现mH2A1.2表现出过表达水平。在癌细胞,抑制HER-2激酶活性,削弱了mH2A1的表达,降低了mH2A1.2诱导的原癌基因ERBB2的转录。
在稳定转染mH2A1.2的癌细胞,染色质免疫共沉淀实验显示,mH2A1.2富集在HER-2的启动子,这表明mH2A1.2具有促进HER-2过表达的作用。
进一步研究表明,进化上保守的mH2A1.2的宏结构域(macro domain),对于HER-2与mH2A1.2的相互作用及mH2A1.2诱导的ERBB2的转录十分必要。
有趣的是,mH2A1.2的宏结构域具有mH2A1.1没有的三核苷酸的插入序列,它可能对HER-2与mH2A1.2的相互作用,对mH2A1.2诱导的ERBB2转录及细胞增生是必不可少的。
Scott K. Kuwada表示,本次发现阐明了mH2A1.2与HER-2之间新的相互作用机制,表明了一个独特的机制,即原癌基因能够广泛的引起癌细胞内基因转录失调

doi: 10.1074/jbc.M112.379412
PMC:
PMID:
The atypical histone macroH2A1.2 interacts with HER-2 in cancer cells
Xiufen Li, Jinqui Kuang, Yi Shen, Martin M. Majer, Chad C. Nelson, Krishna Parsawar, Karen A. Heichman and Scott K. Kuwada
Since HER-2 has been demonstrated in the nuclei of cancer cells we hypothesized that it might interact with transcription factors that activate ERBB2 transcription.macroHistone 2A1 (H2AFY; mH2A1) was found to interact with HER-2 in cancer cells that overexpress HER-2. Of the two human mH2A1 isoforms, mH2A1.2, but not mH2A1.1, interacted with HER-2 in human cancer cell lines.Overexpression of mH2A1.2, but not mH2A1.1, in cancer cells significantly increased HER-2 expression and tumorigenicity. Inhibition of HER-2 kinase activity diminished mH2A1 expression and mH2A1.2-induced ERBB2 transcription in cancer cells.Chromatin immunoprecipitation of mH2A1.2 in cancer cells stably transfected with mH2A1.2 showed enrichment of mH2A1.2 at the HER-2 promoter suggesting a role for mH2A1.2 in driving HER-2 overexpression.The evolutionarily conserved macro domain of mH2A1.2 was sufficient for the interaction between HER-2 and mH2A1.2, and, for mH2A1.2-induced ERBB2 transcription.Within the macro domain of mH2A1.2, a trinucleotide insertion (-eis) sequence not found in mH2A1.1 was essential for the interaction between HER-2 and mH2A1.2 as well as mH2A1.2-induced HER-2 expression and cell proliferation.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#相互作用#
87
#JBC#
58
#癌细胞#
57
#组蛋白#
62
#互作#
77
#HER-2#
61