Eur Heart J:恩格列净对不同射血分数心衰患者的影响
2021-12-10 MedSci原创 MedSci原创
恩格列净对心力衰竭结局的影响程度在射血分数<25%至<65%的患者中具有临床意义,且各组的效应相似,但在射血分数≥65%的患者中有所减弱。
目前,在临床实践中没有任何疗法可以降低不同射血分数范围的心力衰竭患者住院风险。

近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,该研究的目的是评估射血分数对钠-葡萄糖协同转运蛋白2抑制剂恩格列净对心力衰竭结局的影响。

研究人员对EMPEROR-降低和EMPEROR-正常试验(9718名患者;4860名接受恩格列净治疗和4858名接受安慰剂治疗)进行了汇总分析,患者根据射血分数进行分组:<25%(n=999)、25-34%(n=2230)、35-44%(n=1272)、45-54%(n=2260)、55-64%(n=2092)和≥65%(n=865)。评估的结局包括(i)首次因心力衰竭或心血管死亡住院的时间,(ii)至首次心力衰竭住院的时间,(iii)因心力衰竭而住院的总(首次和复发)住院时间,以及(iv)评估的健康状况堪萨斯城心肌病问卷(KCCQ)。
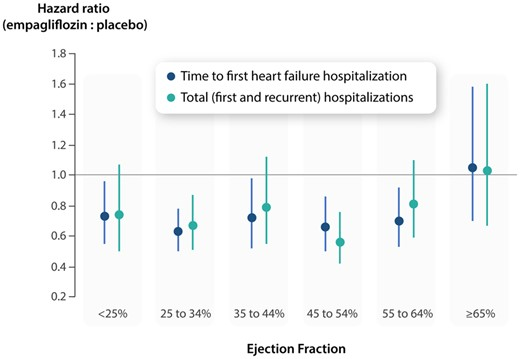
随着射血分数从<25%增加到≥65%,心血管死亡和因心力衰竭住院的风险逐渐下降。恩格列净降低了心血管死亡或心力衰竭住院的风险,主要是通过减少了心力衰竭住院。恩格列净在所有射血分数亚组中将心力衰竭住院风险降低了约30%,对射血分数≥65%的患者效果有所减弱。风险比和95%置信区间为:射血分数<25%:0.73(0.55-0.96);射血分数25-34%:0.63(0.50-0.78);射血分数35-44%:0.72(0.52-0.98);射血分数45-54%:0.66(0.50-0.86);射血分数55-64%:0.70(0.53-0.92);射血分数≥65%:1.05(0.70-1.58)。其它心力衰竭结局和指标,包括KCCQ、具有类似的反应模式。性别并不影响对恩格列净的治疗反应。
由此可见,恩格列净对心力衰竭结局的影响程度在射血分数<25%至<65%的患者中具有临床意义,且各组的效应相似,但在射血分数≥65%的患者中有所减弱。
原始出处:
Javed Butler.et al.Effect of empagliflozin in patients with heart failure across the spectrum of left ventricular ejection fraction.European Heart Journal.2021.https://academic.oup.com/eurheartj/advance-article/doi/10.1093/eurheartj/ehab798/6455932
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习了,谢谢
65
#ART#
61
#心衰患者#
56
#HEART#
54
学习了
80
很实用
84