慢性血栓栓塞性肺动脉高压患者心脏成纤维细胞活化的影像学研究
2021-10-21 刘少飞 MedSci原创
慢性血栓栓塞性肺动脉高压 (CTEPH) 中长期升高的右心室 (RV) 后负荷导致 RV 的适应不良重塑,从而导致 RV 衰竭。 在这个适应过程中,心肌纤维化起着至关重要的作用。

慢性血栓栓塞性肺动脉高压 (CTEPH) 中长期升高的右心室 (RV) 后负荷导致 RV 的适应不良重塑,从而导致 RV 衰竭。 在这个适应过程中,心肌纤维化起着至关重要的作用。 这种结构紊乱会损害 RV 收缩和舒张,并且与 CTEPH 的疾病严重程度密切相关。 由于 RV 纤维化是一个高度动态的过程,因此它可能至少在某个时期是可逆的。 因此,直接评估 CTEPH 中 RV 纤维化的发展可能为及时干预和防止心肌组织的不可逆重塑提供机会。
心脏磁共振 (CMR) 是一种经过临床验证的检测心肌纤维化的技术。 晚期钆增强 (LGE) 可以使用分布到细胞外空间的造影剂来观察纤维化。 T1 映射是一种新兴工具,可以量化图像中每个体素的 T1 弛豫时间。 天然 T1 时间和增强的 T1 时间与心肌纤维化含量显着相关。 此外,结合对比前和对比后的 T1 时间可以计算细胞外体积 (ECV) 。 然而,LGE 和 T1 映射都反映了细胞外基质体积的变化,而不是提供成纤维细胞或胶原蛋白的靶向成像。 此外,虽然 LGE 和 T1 映射已广泛应用于检测各种心脏病中左心室的心肌纤维化,但只有少数研究报告了其用于评估右侧心脏病.
因此,本初步研究的目的如下:(1)评估 CTEPH 患者心脏 68 镓标记的成纤维细胞活化蛋白抑制剂(68 Ga-FAPI-04)摄取的特征和(2)探讨 RV 的相关性 68 Ga-FAPI-04 摄取与临床和 CMR 参数。
研究方法:前瞻性招募了 13 名 CTEPH 患者。所有患者均接受了心脏镓标记的成纤维细胞活化蛋白抑制剂(Ga-FAPI-04)-正电子发射断层扫描/计算机断层扫描(PET/CT)、右心导管插入术和超声心动图检查,其中11例还接受了CMR检查。选择了 13 名对照受试者来确定心脏 Ga-FAPI-04 摄取的正常范围。心脏 Ga-FAPI-04 摄取高于血池被定义为异常。测量右心室 (RV) 的整体和节段最大标准化摄取值 (SUV) 并进一步表示为目标与背景比 (TBR),以左心室侧壁活动为背景。视觉评估晚期钆增强 (LGE),并定量测量天然 T1 时间、增强 T1 时间和细胞外体积 (ECV)。
研究初步结果:10名CTEPH患者(77%)在RV中Ga-FAPI-04摄取异常,主要位于游离壁,明显高于对照组(TBR:2.4 ± 0.9 vs 1.0 ± 0.1,P < 0.001) . TBR与RV壁的厚度(r = 0.815,P = 0.001)呈正相关,与RV分数面积变化(RVFAC)(r = - 0.804,P = 0.0001)和三尖瓣环外旋(三尖瓣环外旋)呈负相关= - 0.678,P = 0.011)。 Ga-FAPI-04 活性与 CMR 成像参数之间未发现相关性。
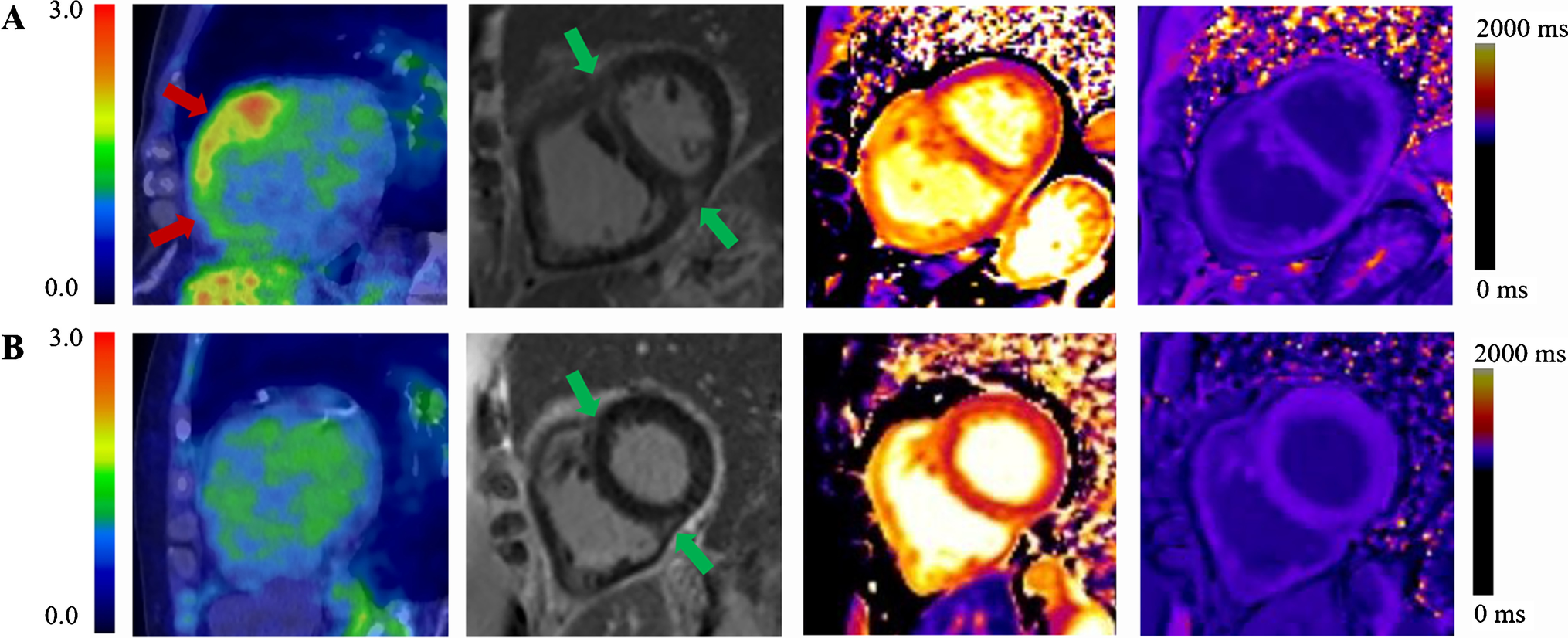
结论:通过 Ga-FAPI-04 成像测量的 CTEPH 中的成纤维细胞活化主要位于 RV 游离壁。增强的成纤维细胞活化反映了 RV 壁的增厚和 RV 收缩功能的降低。
Chen BX, Xing HQ, Gong JN, Guo XJ, Xi XY, Yang YH, Huo L, Yang MF. Imaging of cardiac fibroblast activation in patients with chronic thromboembolic pulmonary hypertension. Eur J Nucl Med Mol Imaging. 2021 Oct 15. doi: 10.1007/s00259-021-05577-9. Epub ahead of print. PMID: 34651221.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#动脉高压#
102
#肺动脉高压患者#
126
#心脏成纤维细胞#
128
#成纤维细胞#
128
#纤维细胞#
108