C3肾小球病的治疗或迎重大突破!Iptacopan显示出希望
2020-10-27 Allan MedSci原创
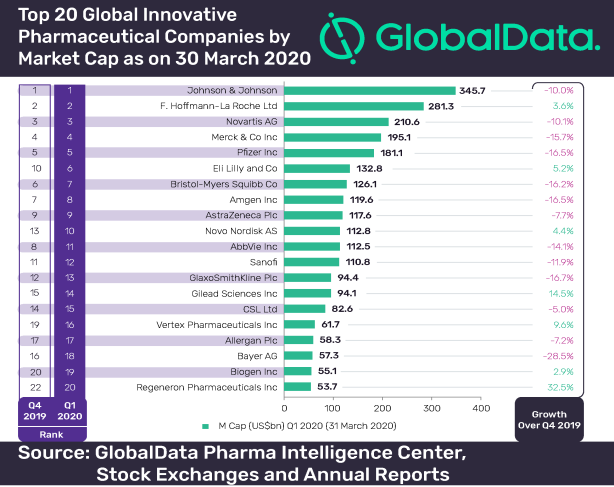
在一项II期研究中,诺华的肾脏疾病候选药物iptacopan的显示出治疗C3肾小球病的希望。
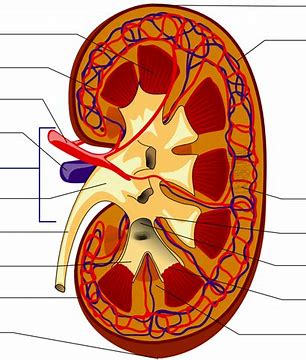
C3肾小球病(C3G)是新提出的肾脏疾病分类, 是指一些罕见的肾炎, 包括致密物沉积病、C3肾小球肾炎和CFHR5肾病等。C3肾小球病具有相同的病因, 即补体旁路途径的异常调节, 有时伴基因缺陷或自身抗体异常。
在一项II期研究中,诺华的肾脏疾病候选药物iptacopan的显示出治疗C3肾小球病的希望。结果显示,与12例患者的基线值相比,该药物在12周后可显著降低49%的蛋白尿(蛋白尿提示肾脏中存在炎症)。这些数据还强调了iptacopan能够强烈和特异性地抑制替代补体途径,从而针对该疾病的根本原因,并可能为C3G患者提供急需的治疗选择。
欧洲药品管理局(EMA)已授予iptacopan治疗C3G的PRIME称号,EMA还授予了iptacopan治疗IgA肾病(IgAN)的孤儿药称号。除了C3G以外,iptacopan还用于许多其他肾脏疾病,如非典型溶血性尿毒症综合征和膜性肾病。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#C3肾小球病#
51
#TAC#
43
学习了
67
#TACO#
40
学习了
94
很受益
88
了解
94