J Thorac Oncol:肥胖NSCLC患者的术后生存更优?
2017-08-28 肿瘤资讯编辑部 肿瘤资讯
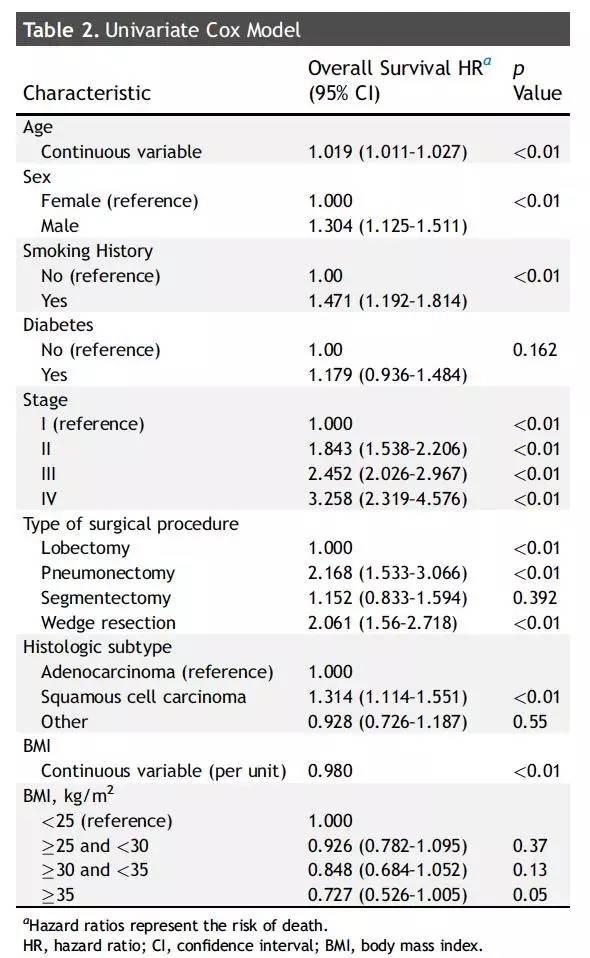
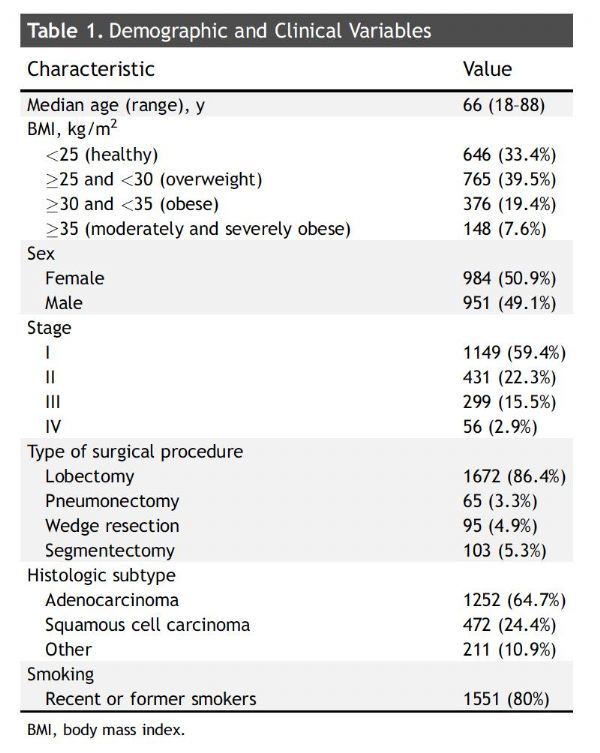
肥胖会增加很多癌症的发病风险。近年来的研究显示,肥胖还会增加癌症患者的死亡风险,如消化道肿瘤,乳腺癌等。然而,肥胖与肺癌患者的预后关系却不尽相同。近日,一项来自MD. Anderson的回顾性研究,分析了接受手术治疗的NSCLC患者,肥胖与患者预后的关系。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#THORAC#
71
#SCLC患者#
0
#Oncol#
100
#NSCLC患者#
65
学习了很多先进的医疗技术
77
BMI的OR为0.977.虽然P值有意义.但是这个值太接近1.临床意义并不大
98
文章很好.值得分享
79
学习了.谢谢
89
高级的实验吧
74
学习了谢谢分享
47